Topic
The Achilles tendon, also known as the calcaneal tendon, is the strongest and thickest tendon in the human body. It connects the gastrocnemius, soleus, and plantaris muscles to the posterior surface of the calcaneus, forming the primary mechanism for plantarflexion of the ankle.
Its superficial location and heavy mechanical load during running, jumping, and walking make it highly susceptible to tendinopathy, partial tears, and complete ruptures. Clinically, rupture of the Achilles tendon is one of the most common tendon injuries in athletes and active individuals.
Synonyms
-
Calcaneal tendon
-
Tendo calcaneus
Origin, Course, and Insertion
-
Origin: Formed by the conjoined tendinous fibers of the gastrocnemius, soleus, and occasionally the plantaris muscle
-
Course: Descends vertically along the posterior aspect of the leg, forming a thick, fibrous band
-
Insertion: Posterior surface of the calcaneus (middle third), into the calcaneal tuberosity
Tendon Attachments
-
Merges with fibers of the gastrocnemius and soleus approximately halfway down the leg
-
Passes posterior to the ankle joint without a synovial sheath but surrounded by paratenon, which facilitates gliding
-
Inserts into the calcaneal tuberosity, sometimes blending with the plantar fascia
Relations
-
Anteriorly: Subtendinous bursa, posterior surface of the calcaneus
-
Posteriorly: Skin and subcutaneous tissue
-
Medially: Flexor hallucis longus tendon
-
Laterally: Fibular tendons (peroneal tendons)
-
Superiorly: Gastrocnemius and soleus muscle bellies
-
Inferiorly: Calcaneal insertion, continuous with plantar fascia
Function
-
Plantarflexion: Primary plantarflexor of the ankle, essential for walking, running, and jumping
-
Knee–ankle coordination: Acts across the ankle joint and indirectly across the knee via gastrocnemius
-
Propulsion: Provides explosive force during sprinting and leaping
-
Stability: Helps maintain posture and balance by resisting dorsiflexion forces
Clinical Significance
-
Tendinopathy: Chronic overuse leads to degeneration, thickening, and pain (common in runners)
-
Partial tears: Cause focal pain and weakness but may still allow limited function
-
Complete rupture: Sudden loss of plantarflexion strength, often accompanied by an audible “pop”
-
Bursitis: Inflammation of retrocalcaneal or subcutaneous bursa adjacent to tendon
-
Surgical relevance: Repair techniques vary; early diagnosis improves outcomes
-
Imaging role: MRI and CT are critical for diagnosis, staging, and preoperative planning
MRI Appearance
-
T1-weighted images:
-
Normal tendon: uniformly low signal (dark band), surrounded by intermediate signal paratenon
-
Partial tear: focal intermediate-to-bright signal within tendon fibers
-
Complete rupture: gap in tendon continuity filled with intermediate signal hematoma
-
-
T2-weighted images:
-
Normal tendon: low signal, darker than on T1
-
Tendinopathy: focal or diffuse high signal intensity within thickened tendon
-
Partial tears: hyperintense linear defects extending into tendon substance
-
Complete rupture: high-signal fluid gap at site of discontinuity
-
-
STIR (Short Tau Inversion Recovery):
-
Normal tendon: dark
-
Pathology: bright hyperintense areas indicating edema, inflammation, or rupture-associated fluid
-
-
Proton Density Fat-Saturated (PD FS):
-
Normal tendon: homogeneously dark
-
Pathology: bright signal clefts or diffuse hyperintensity in tendinopathy, small partial tears, or peritendinous inflammation
-
-
T1 Fat-Sat Post-Contrast:
-
Normal tendon: minimal or no enhancement
-
Tendinopathy: mild enhancement of paratenon
-
Postoperative or inflammatory changes: strong linear or diffuse enhancement
-
CT Appearance
Non-Contrast CT:
-
Tendon visible as a dense, thick band posterior to ankle
-
Useful in identifying calcifications, ossifications, or chronic degenerative changes
-
Indirect rupture signs: tendon discontinuity, surrounding soft-tissue swelling
Post-Contrast CT (standard):
-
Normal tendon enhances minimally
-
Pathology: paratenon inflammation or peritendinous soft-tissue enhancement
-
Less sensitive than MRI but valuable when MRI is contraindicated
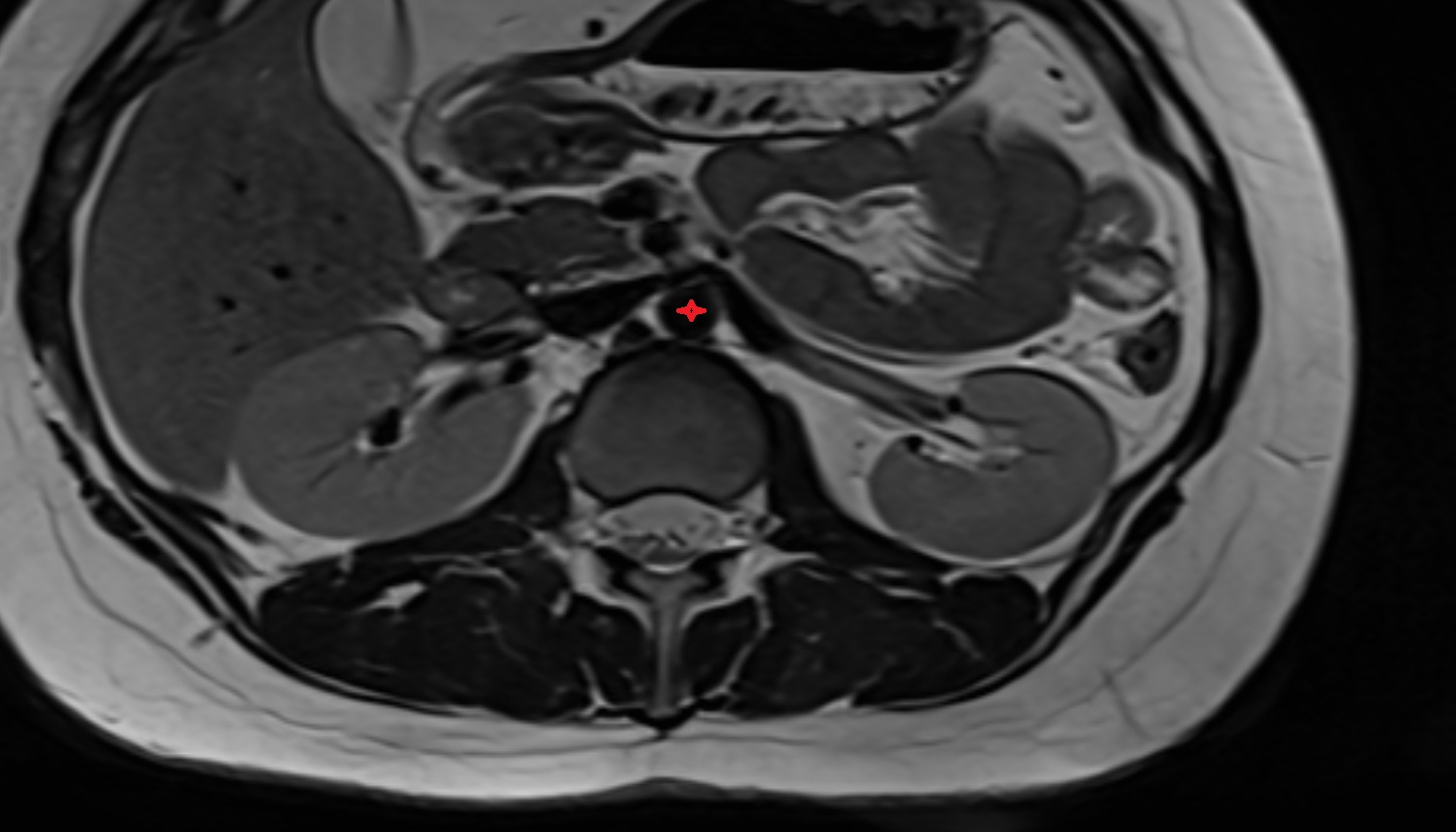
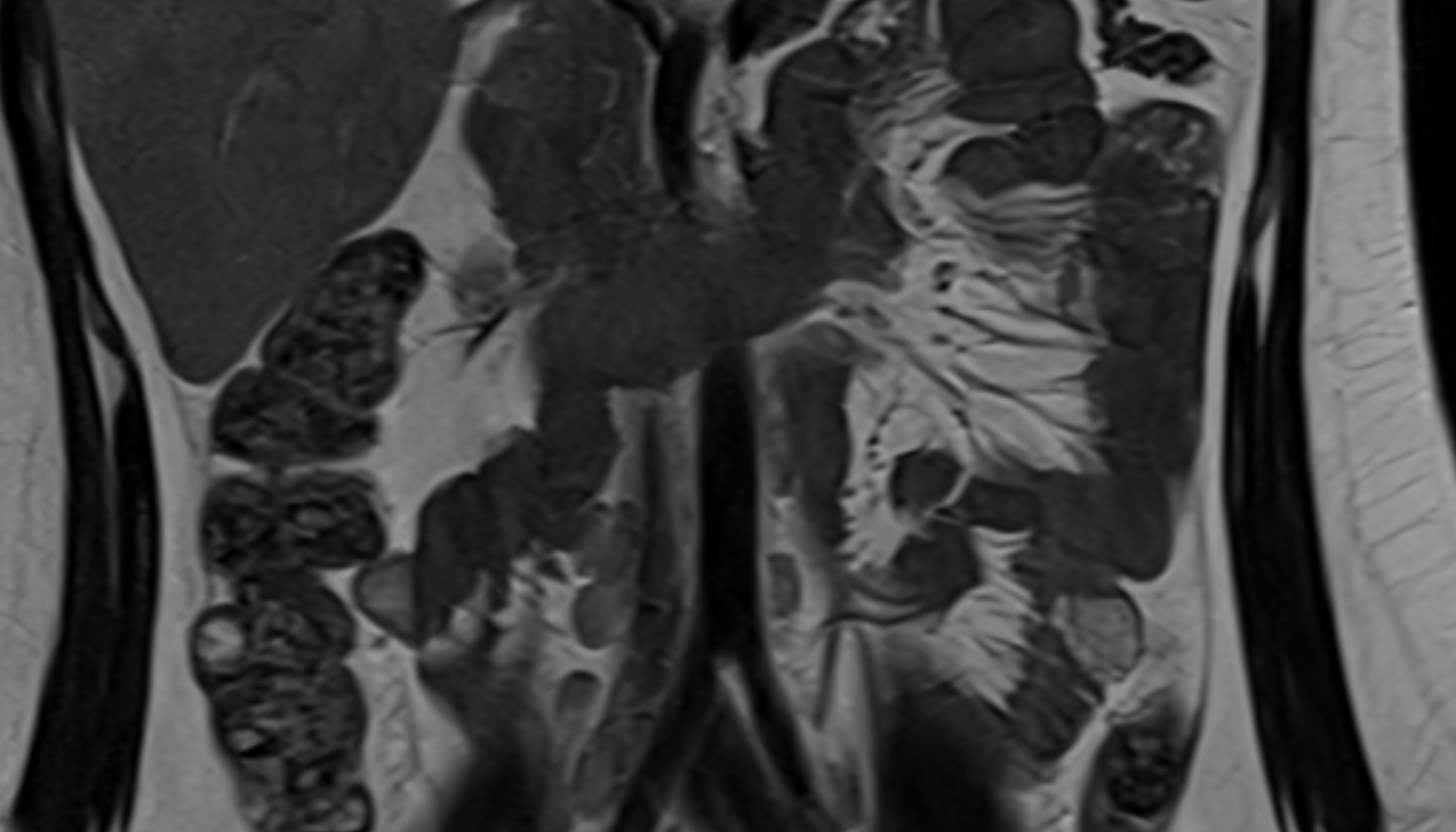
MRI image

MRI image

MRI image

MRI image

MRI image

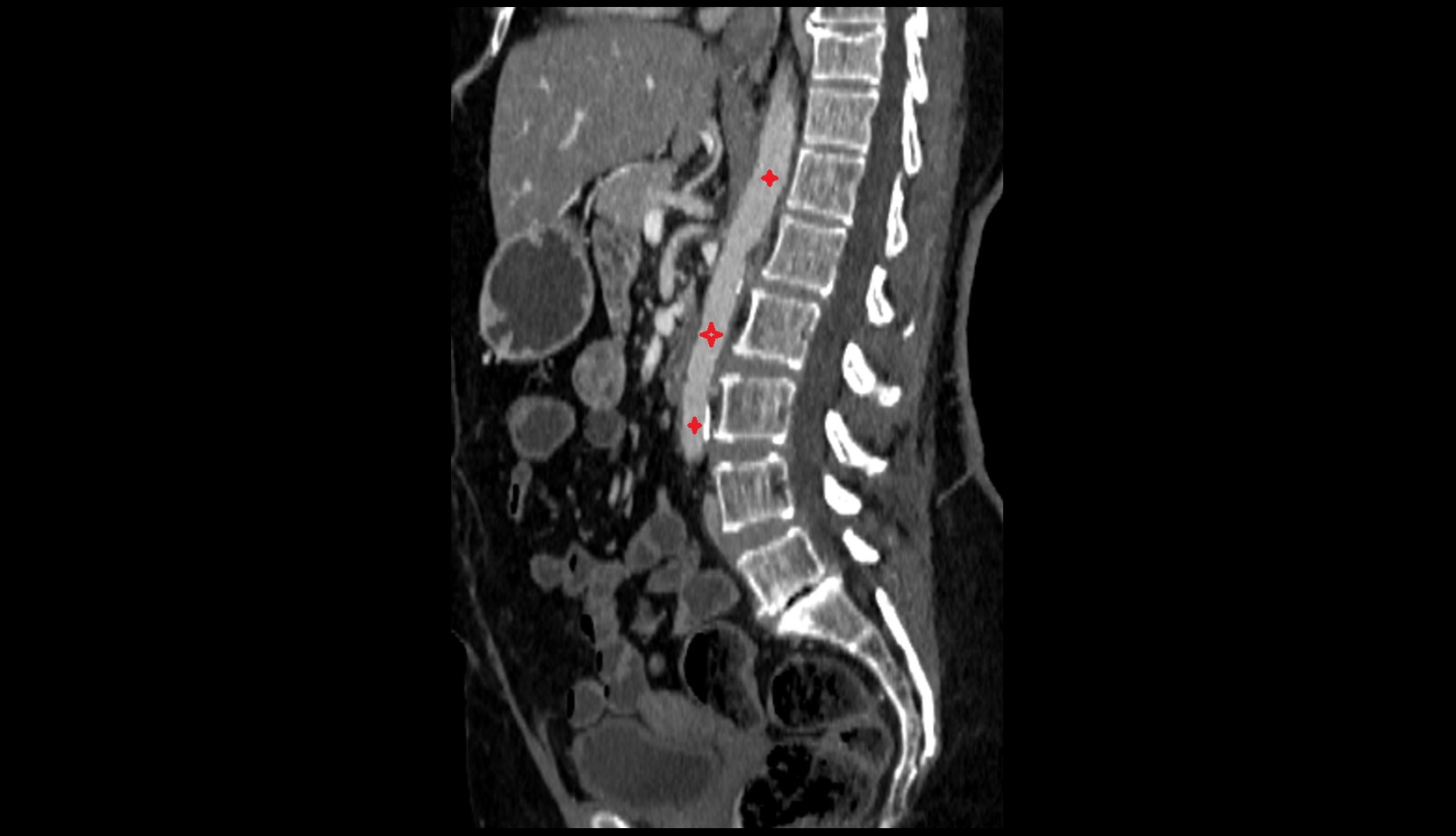
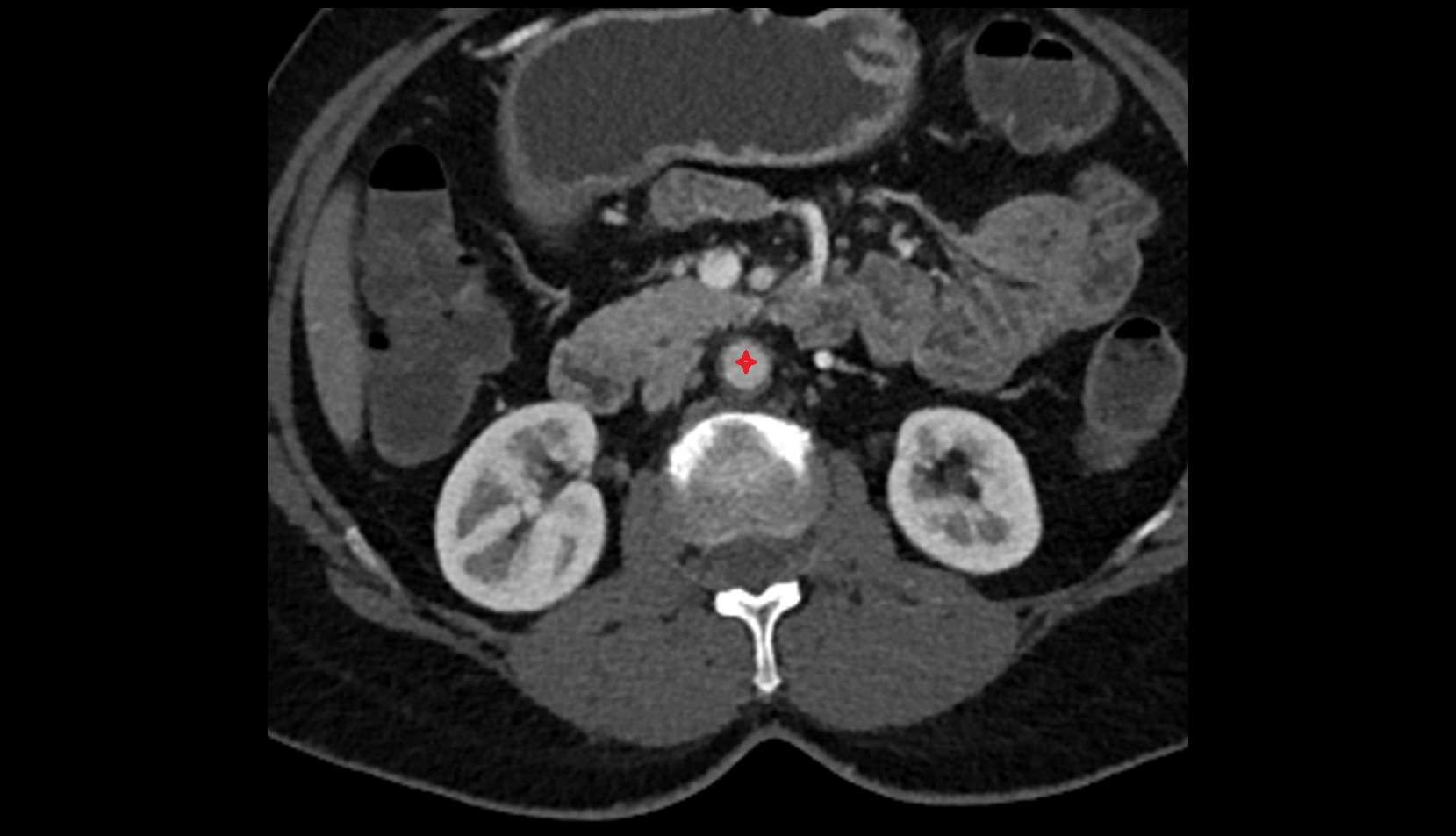
CT image