Topic
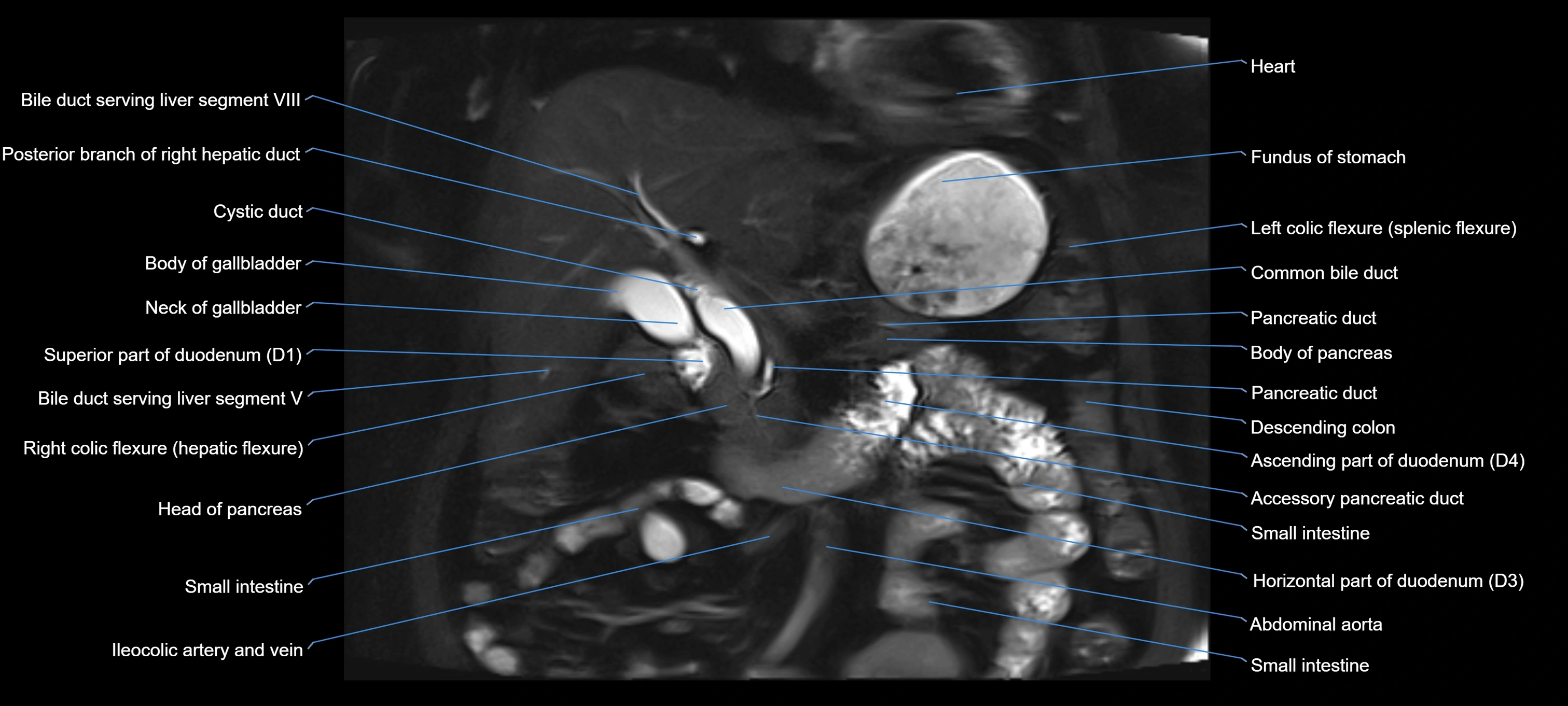
The accessory pancreatic duct, also known as the duct of Santorini, is a secondary pancreatic duct that usually drains the anterior portion of the head of the pancreas. It is the embryologic remnant of the dorsal pancreatic duct system. In many individuals, it persists and provides an additional drainage pathway into the duodenum through the minor duodenal papilla, located proximal and superior to the major papilla.
Although often small or functionally insignificant, it is clinically important because its patency and variations can influence pancreatic drainage and predispose to certain pancreaticobiliary disorders.
Synonyms
-
Duct of Santorini
-
Minor pancreatic duct
-
Accessory duct of the pancreas
Origin, Course, and Termination
-
Origin: Branches from the main pancreatic duct (duct of Wirsung), typically in the head of the pancreas
-
Course: Runs superior and anterior within the pancreatic head toward the minor papilla
-
Termination: Opens into the minor duodenal papilla, about 2 cm proximal to the major papilla in the second part of the duodenum
Relations
-
Anteriorly: Duodenal wall (second part)
-
Posteriorly: Head of the pancreas and main pancreatic duct
-
Superiorly: Common bile duct
-
Inferiorly: Main pancreatic duct (duct of Wirsung) and major papilla
Function
-
Provides an accessory drainage pathway for pancreatic juice into the duodenum
-
In some cases, remains the primary drainage route if the main pancreatic duct is atretic or stenosed
-
Acts as a safety mechanism to reduce intrapancreatic ductal pressure
Clinical Significance
-
Pancreas divisum: Failure of fusion of dorsal and ventral pancreatic ducts; the accessory duct may become the dominant drainage pathway, potentially predisposing to recurrent pancreatitis
-
Minor papilla obstruction: May lead to impaired drainage and pancreatitis
-
Anatomical variants: Varying size and patency can complicate surgical or endoscopic interventions
-
Endoscopic retrograde cholangiopancreatography (ERCP): Identification is critical during pancreatic duct cannulation
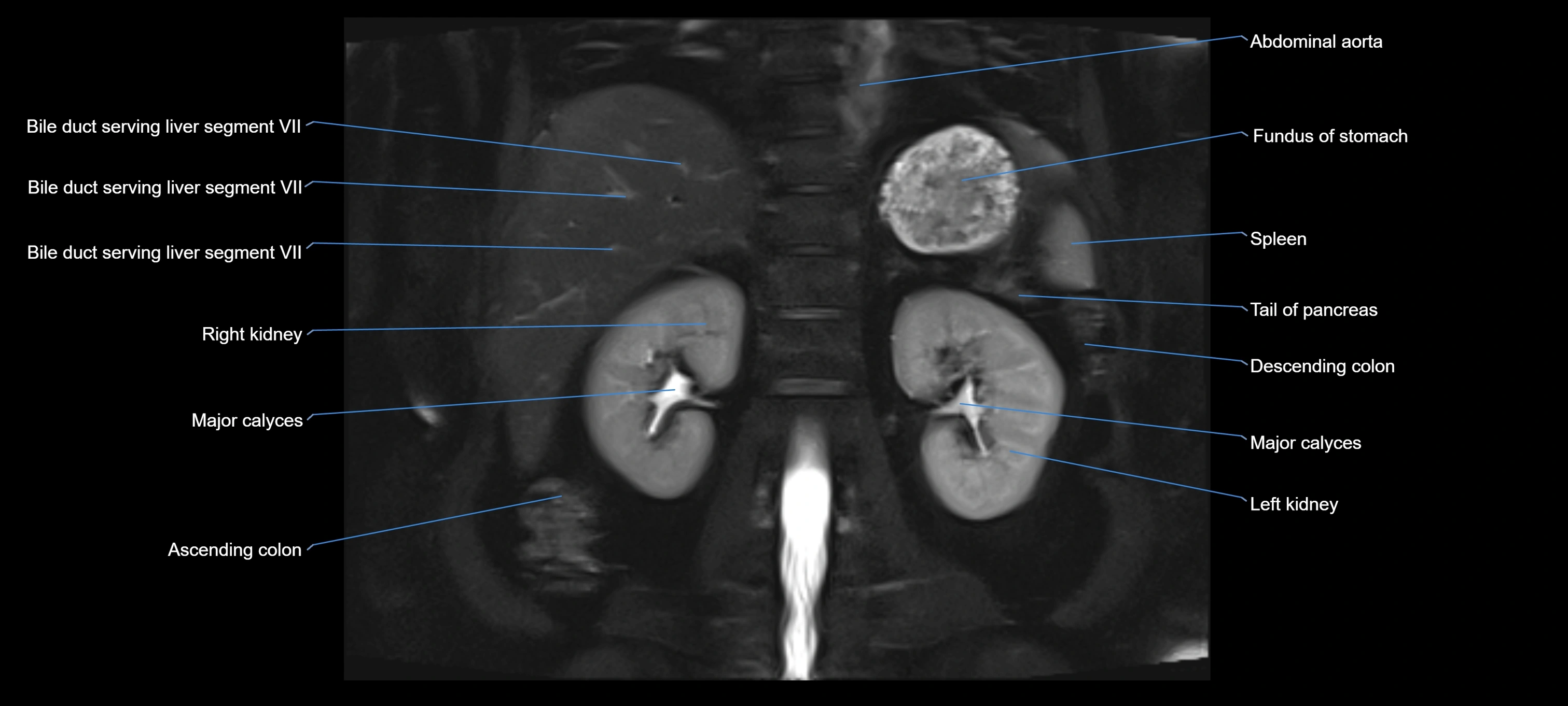
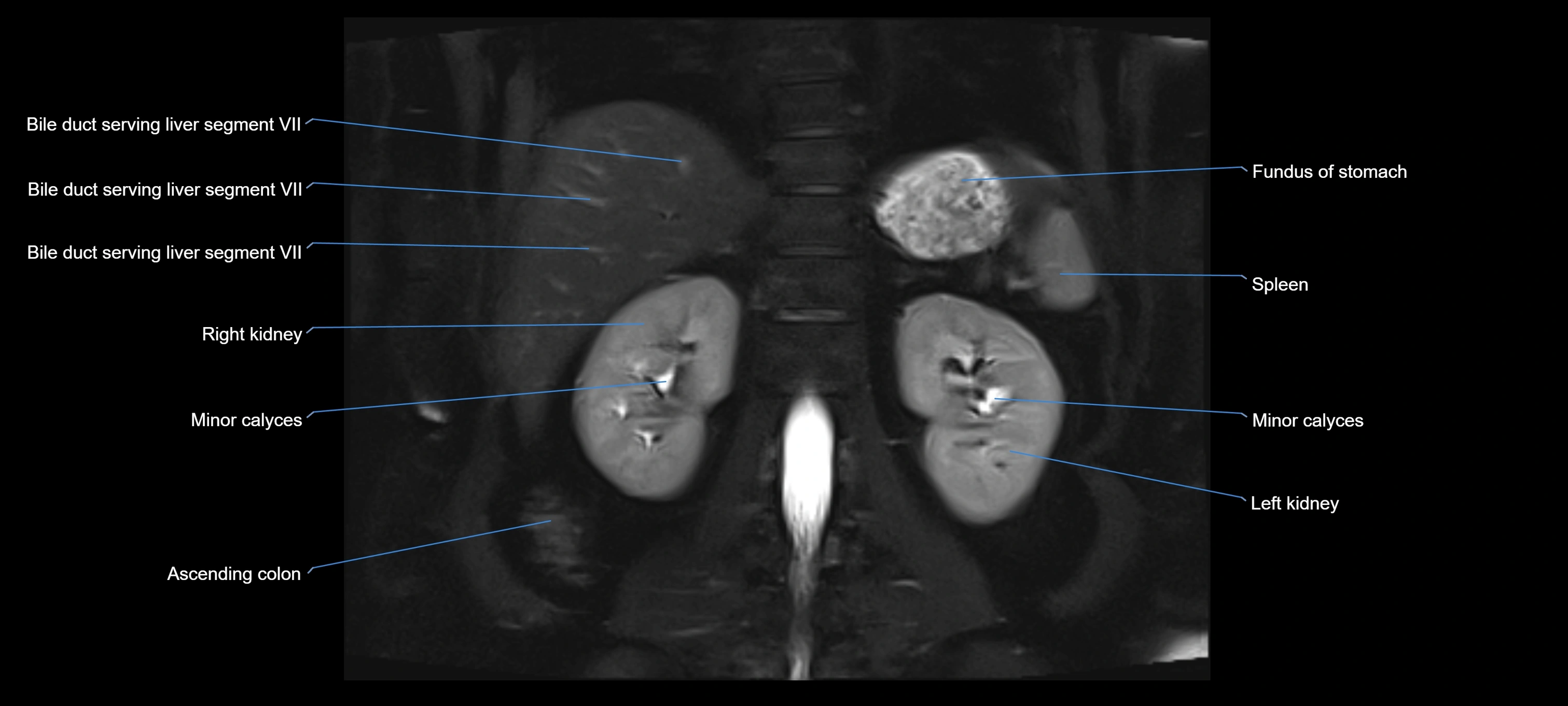
MRI Appearance
T1-weighted images:
-
Not typically visualized unless dilated; appears as low signal tubular structure if seen
-
Surrounding pancreatic parenchyma shows intermediate signal
T2-weighted images:
-
Duct fluid appears bright
-
Accessory duct seen as a fine high-signal tubular structure in pancreatic head
STIR (Short Tau Inversion Recovery):
-
Duct fluid remains bright
-
Surrounding fat suppressed, improving duct conspicuity
T1 Fat-Sat Post-Contrast:
-
Normal duct does not enhance
-
Surrounding inflammatory or neoplastic changes may enhance
T2 Fat-Saturated HASTE (single-shot):
-
Accessory duct: bright, thin linear structure in pancreatic head
-
Stones, strictures, or air bubbles appear as dark filling defects
-
Excellent for rapid evaluation of duct patency
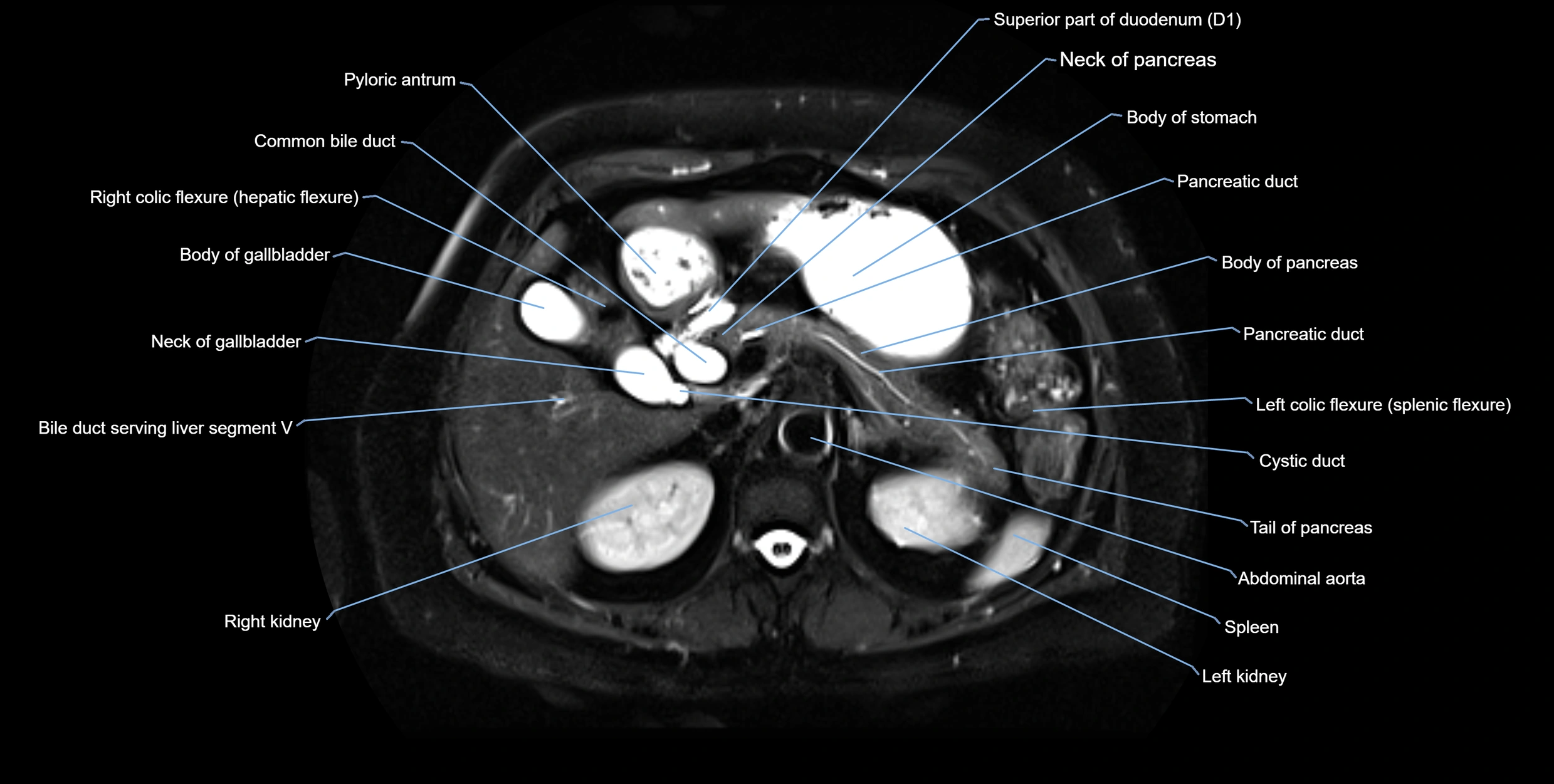
T2 TSE Fat-Saturated 3D (MRCP sequence):
-
Duct visualized as a continuous bright tubular structure joining or parallel to the main pancreatic duct
-
Allows 3D reconstruction of ductal anatomy and variants
-
Excellent for diagnosis of pancreas divisum
Thick-slab T2 Fat-Saturated HASTE:
-
Shows the accessory duct as part of the biliary–pancreatic system in a projectional image
-
Highlights communication with main pancreatic duct and opening into the minor papilla
-
Filling defects (stones, strictures) seen as dark spots within bright fluid
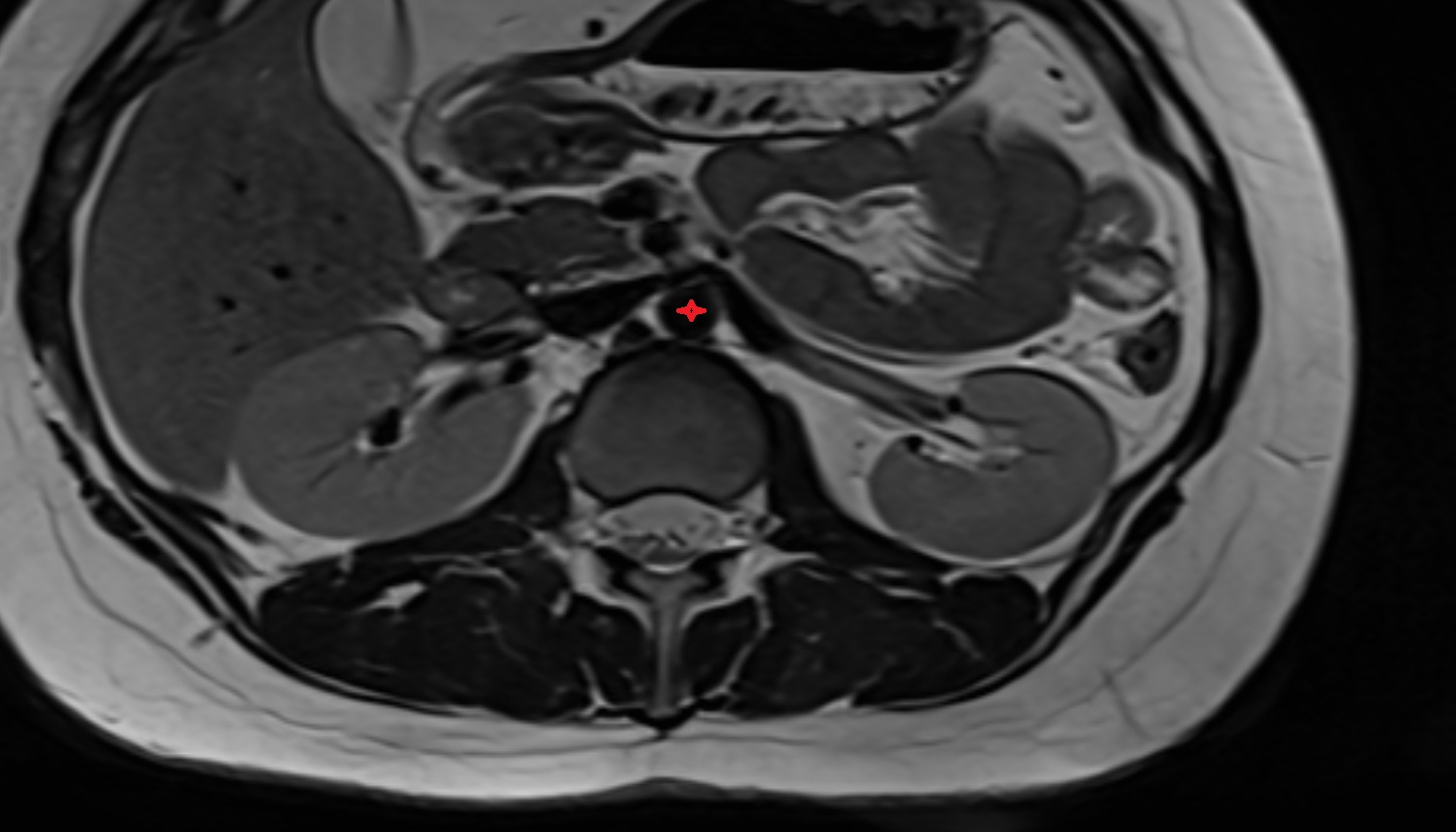
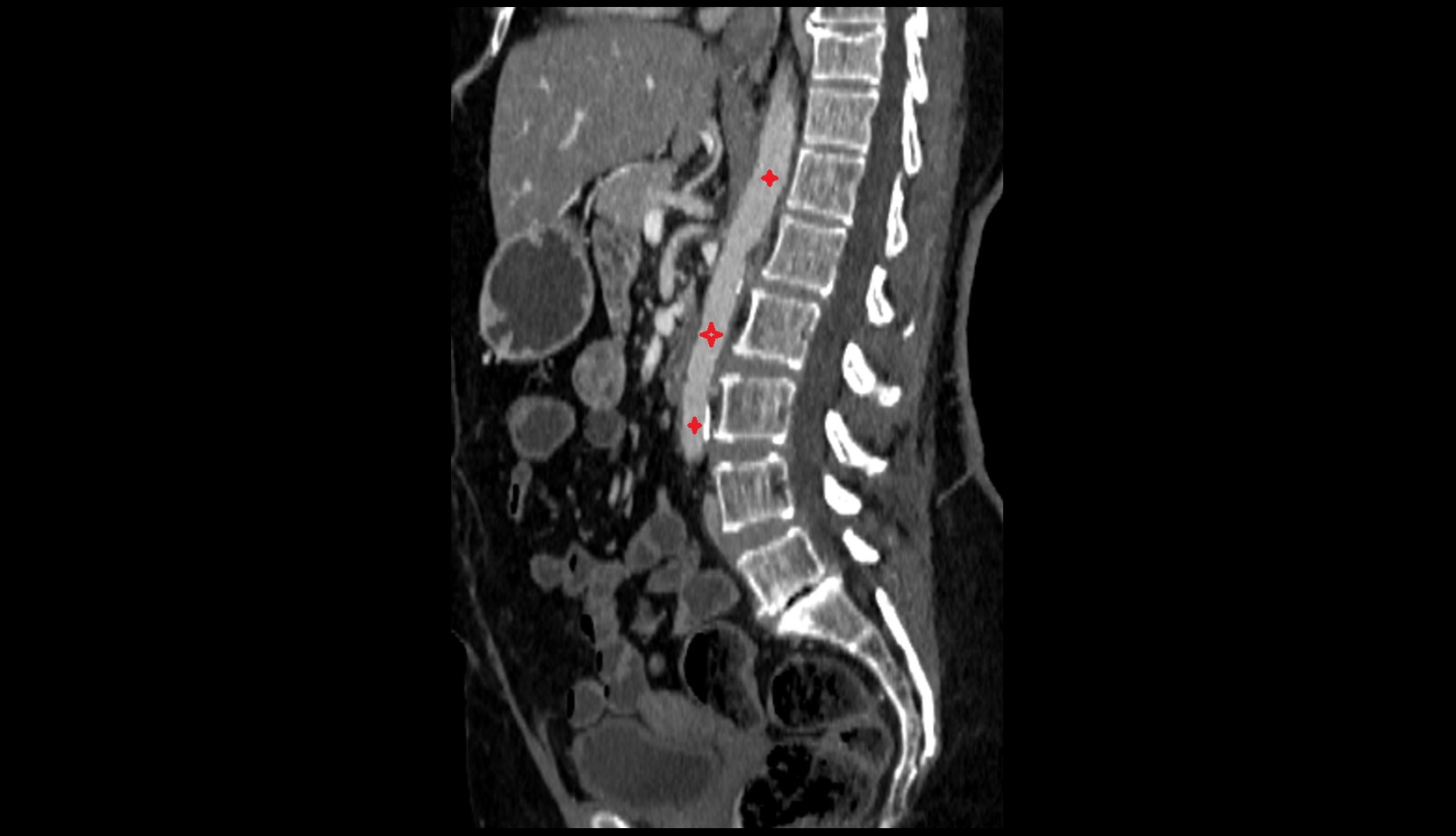
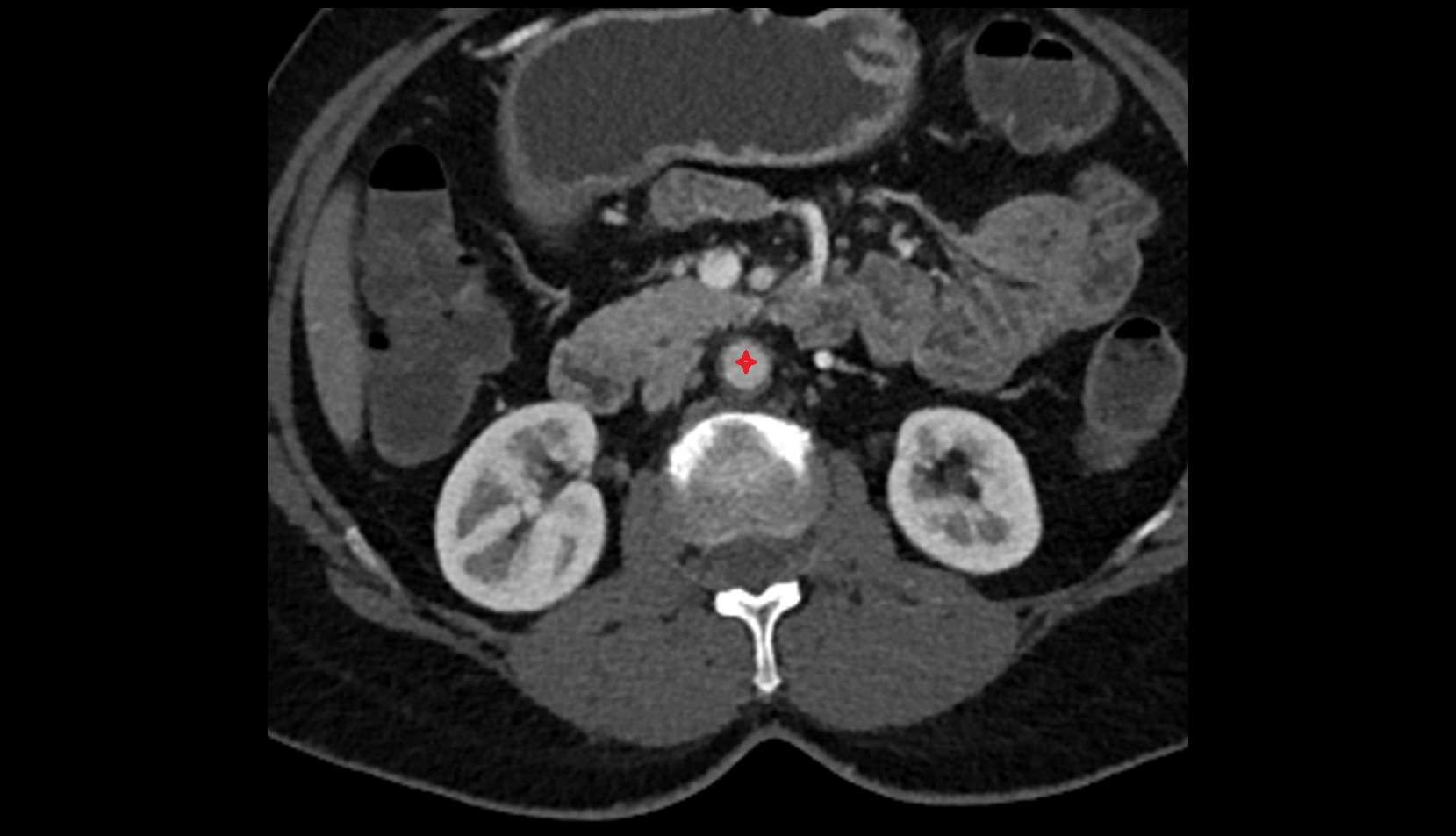
CT Appearance
Non-Contrast CT:
-
Normally not visible unless dilated
-
Appears as a fine low-attenuation tubular structure in pancreatic head when dilated
-
Calcified stones may be detected if present
Post-Contrast CT:
-
Duct lumen remains unenhanced, surrounded by enhancing pancreatic parenchyma
-
Dilatation or obstruction becomes more conspicuous
-
Tumor or inflammatory mass may cause ductal cut-off or narrowing
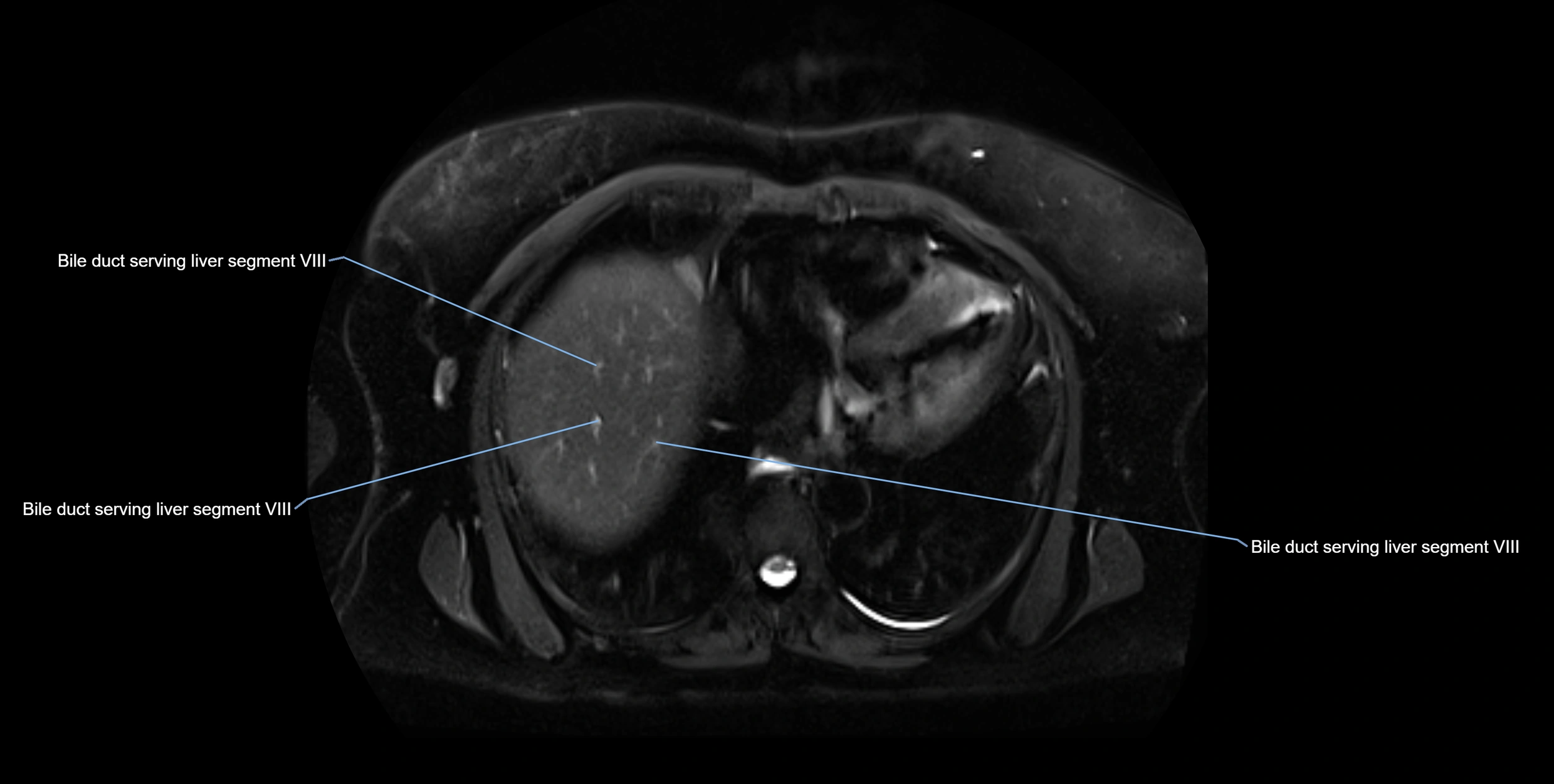
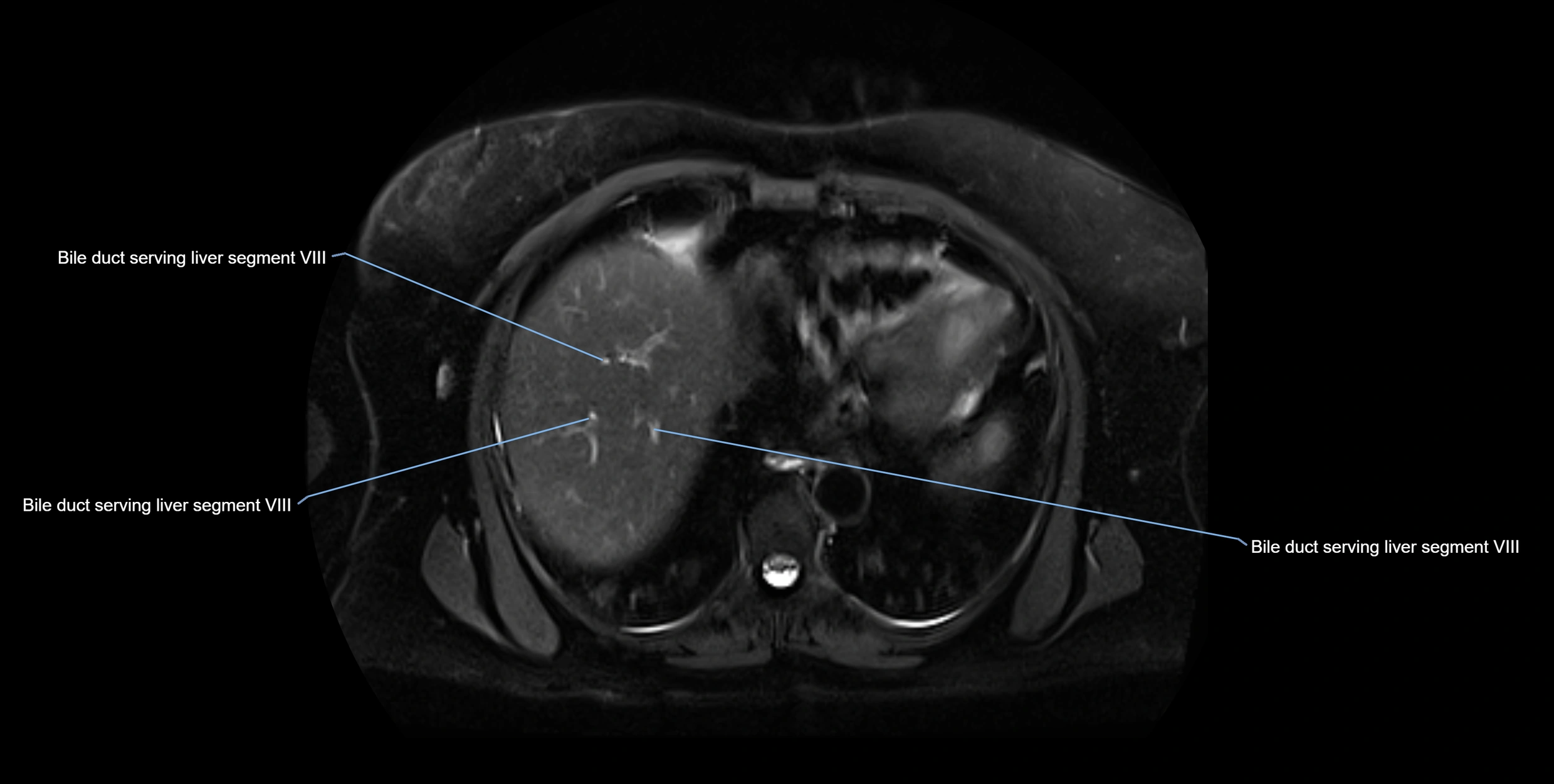
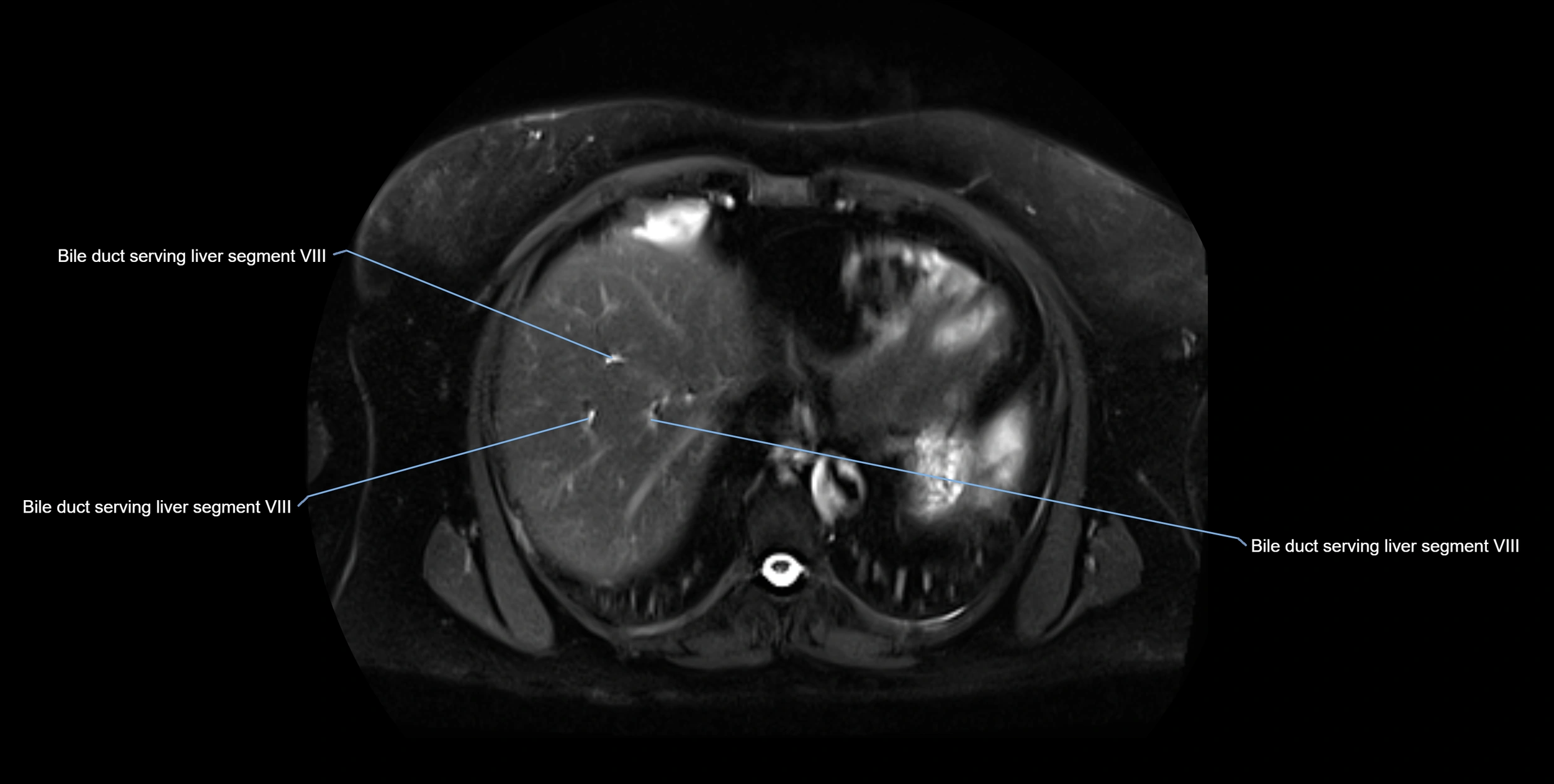
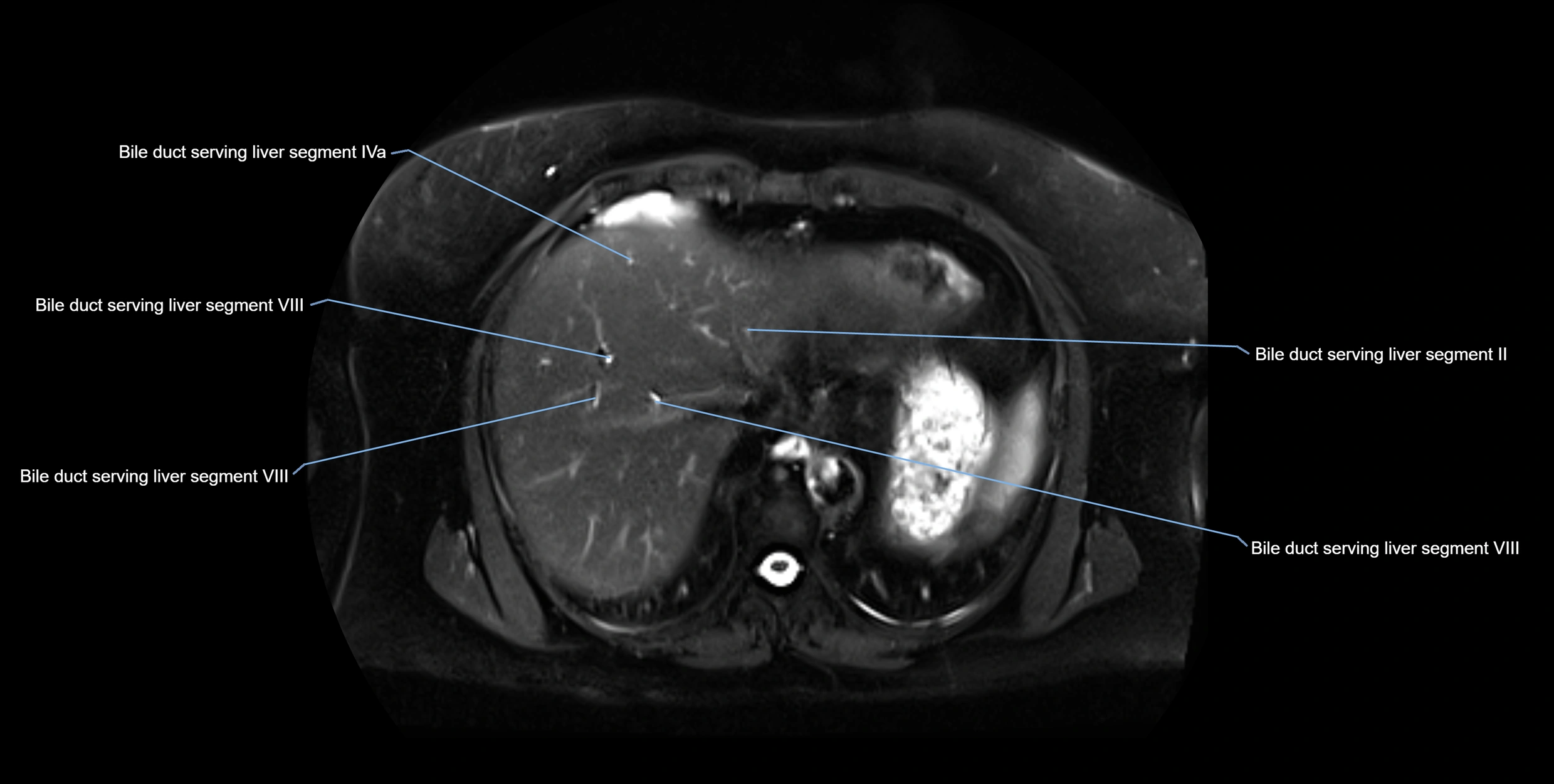
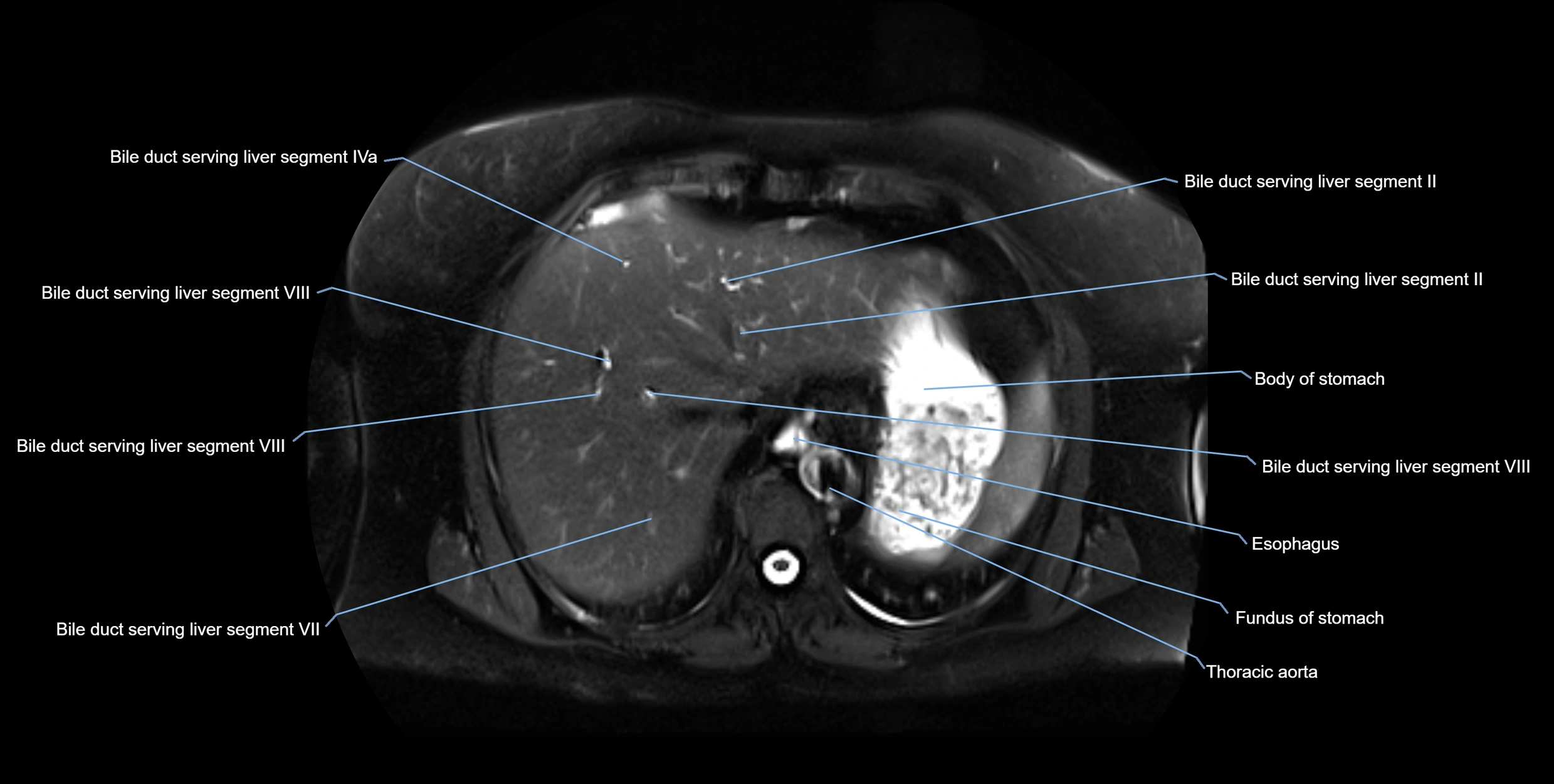
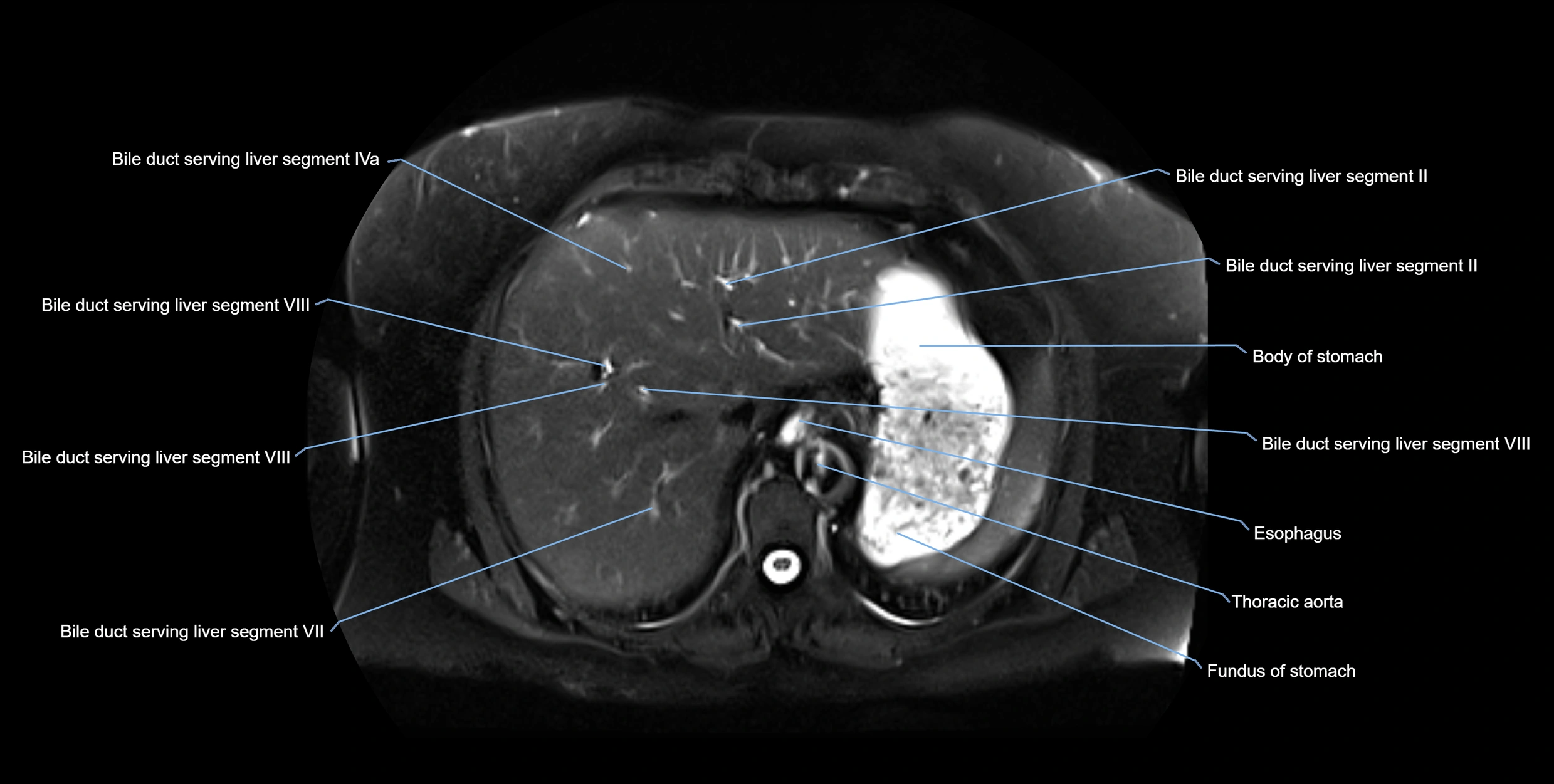
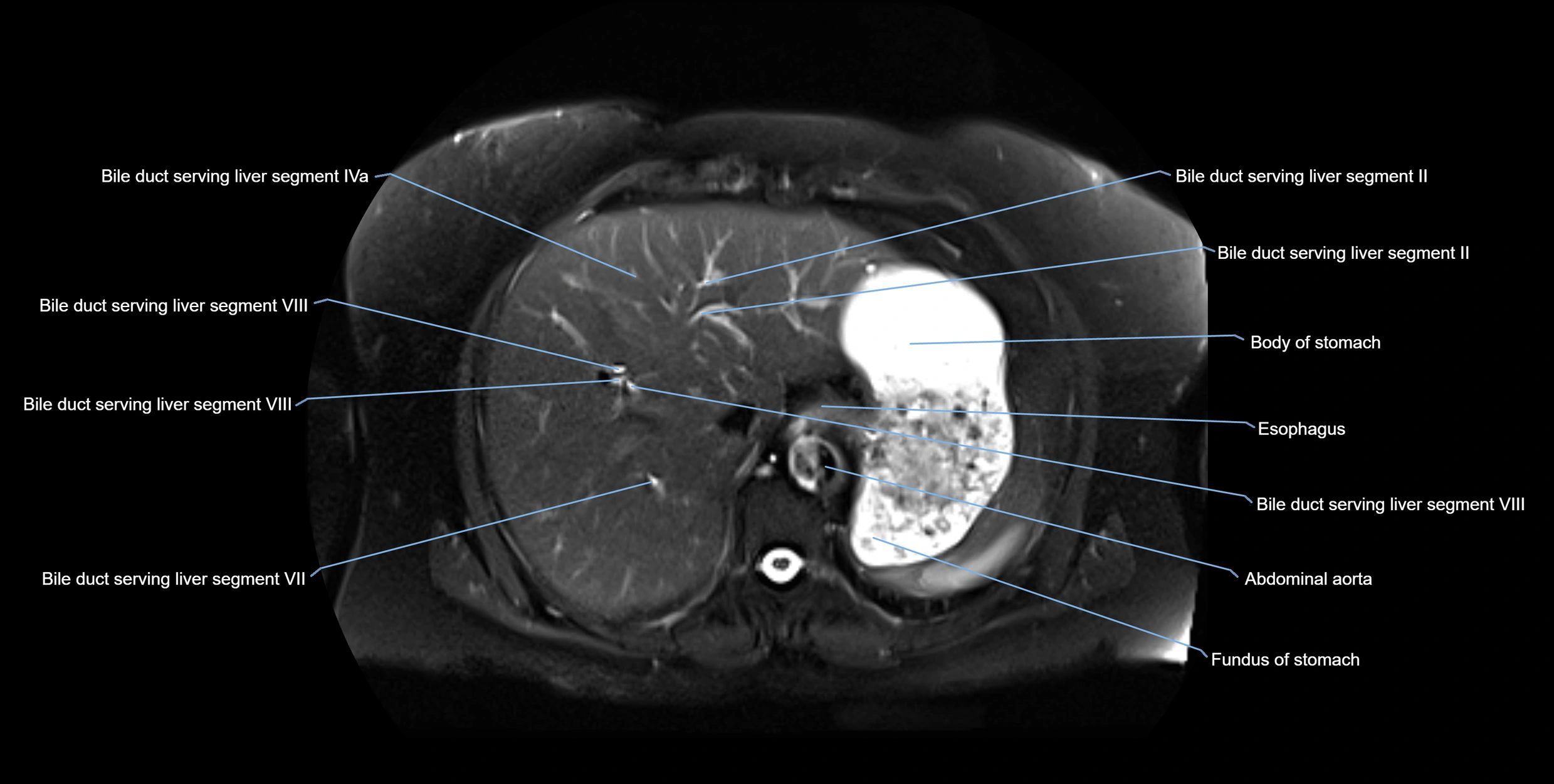
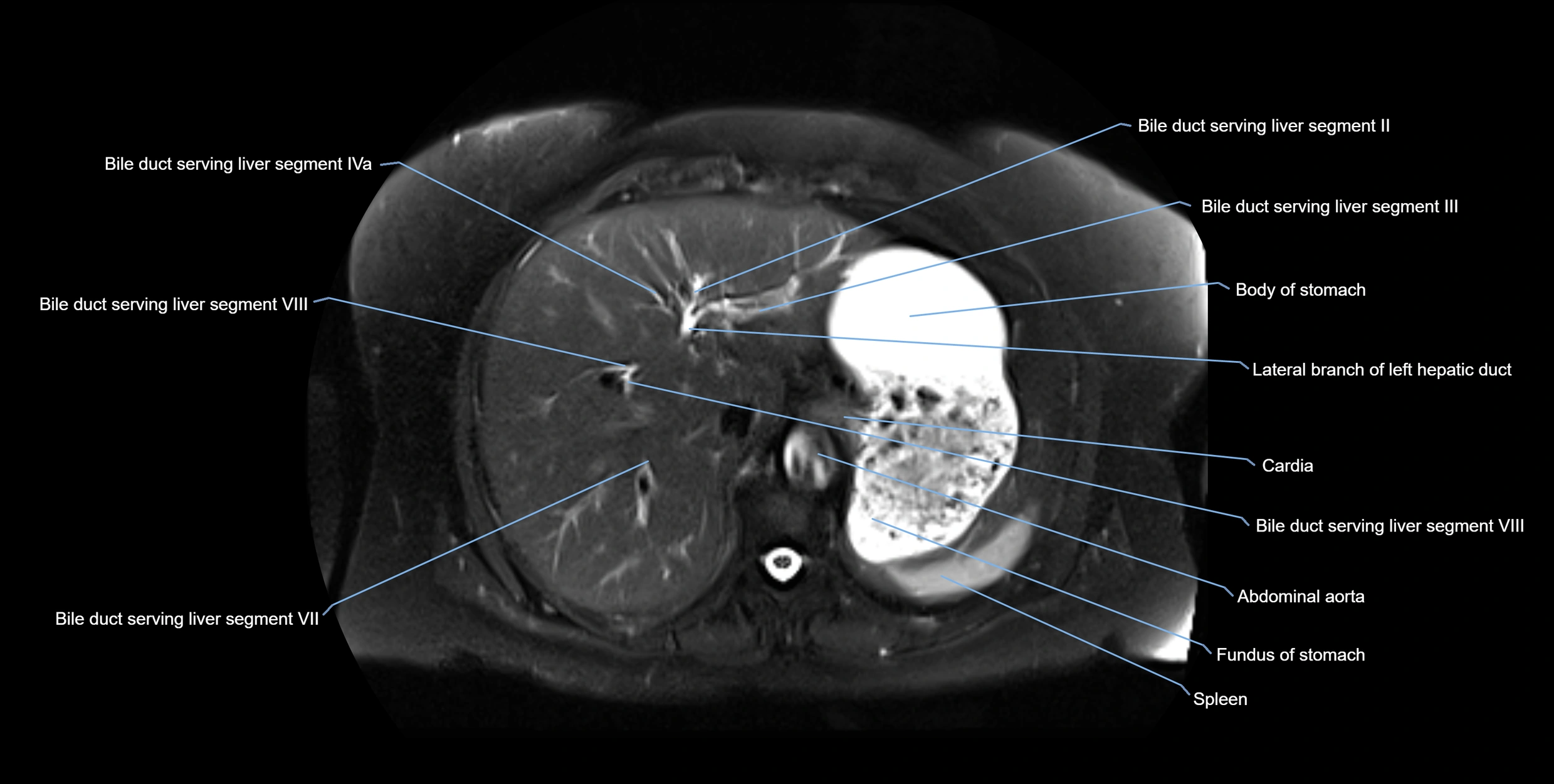
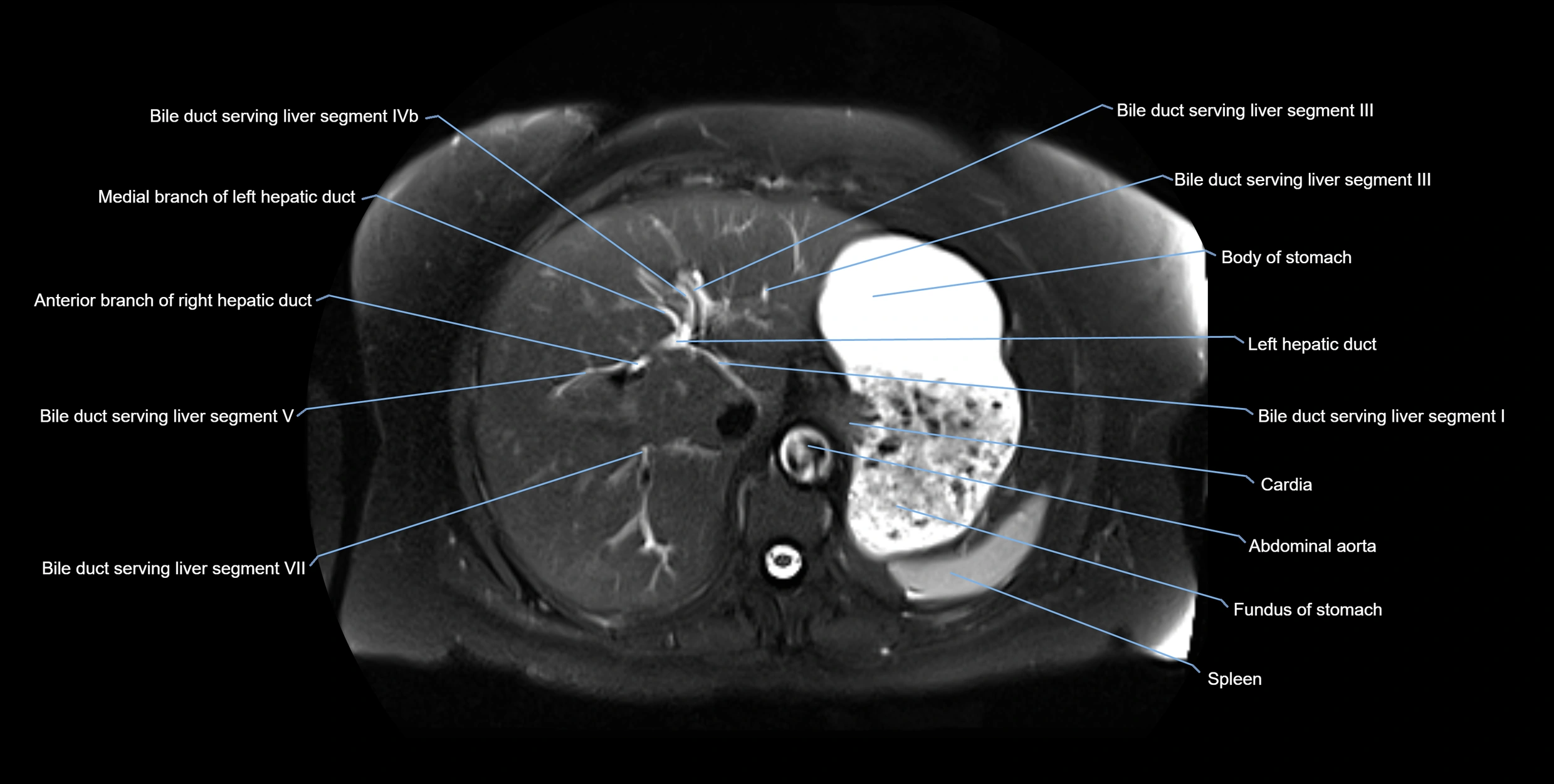
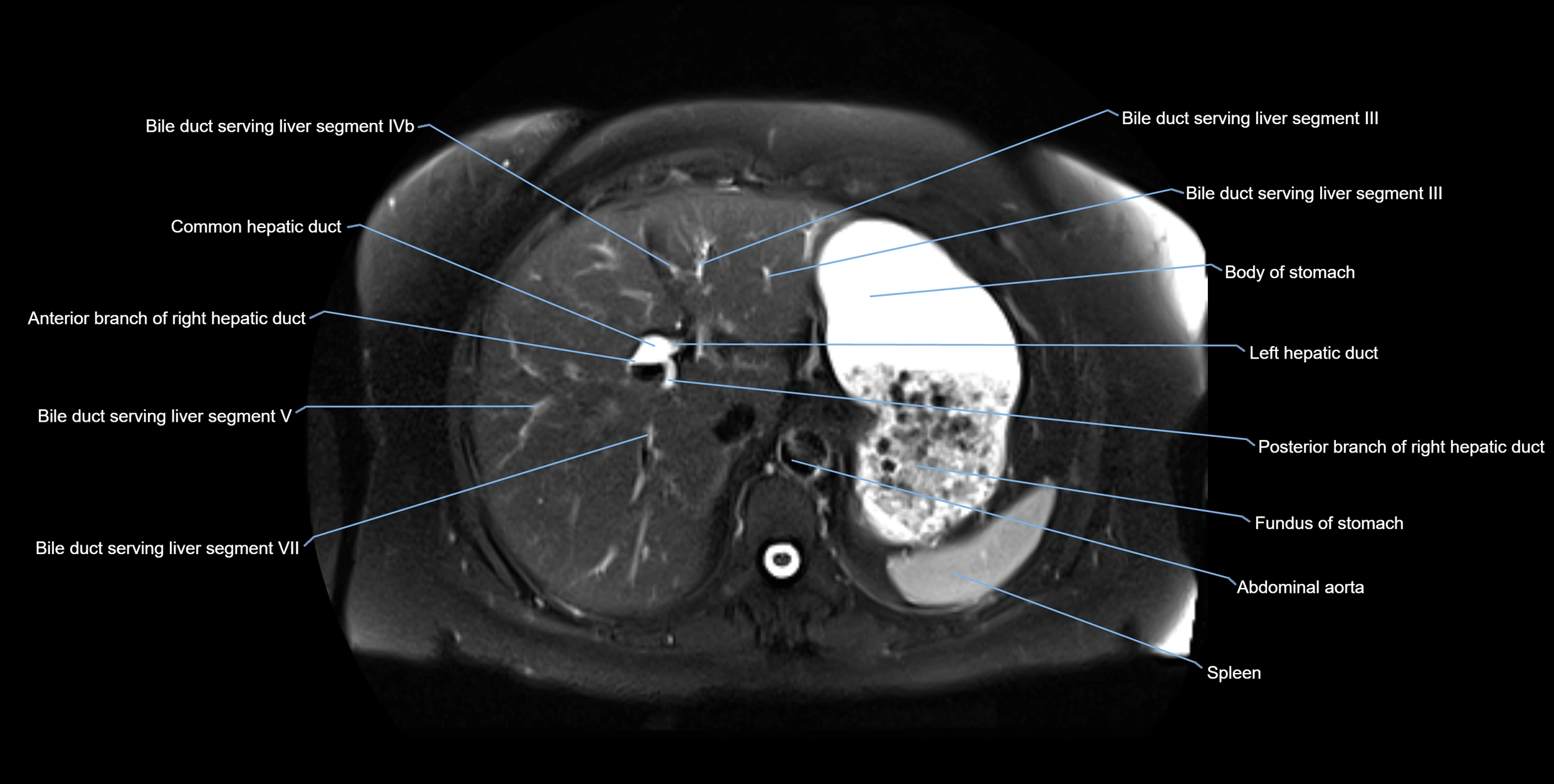
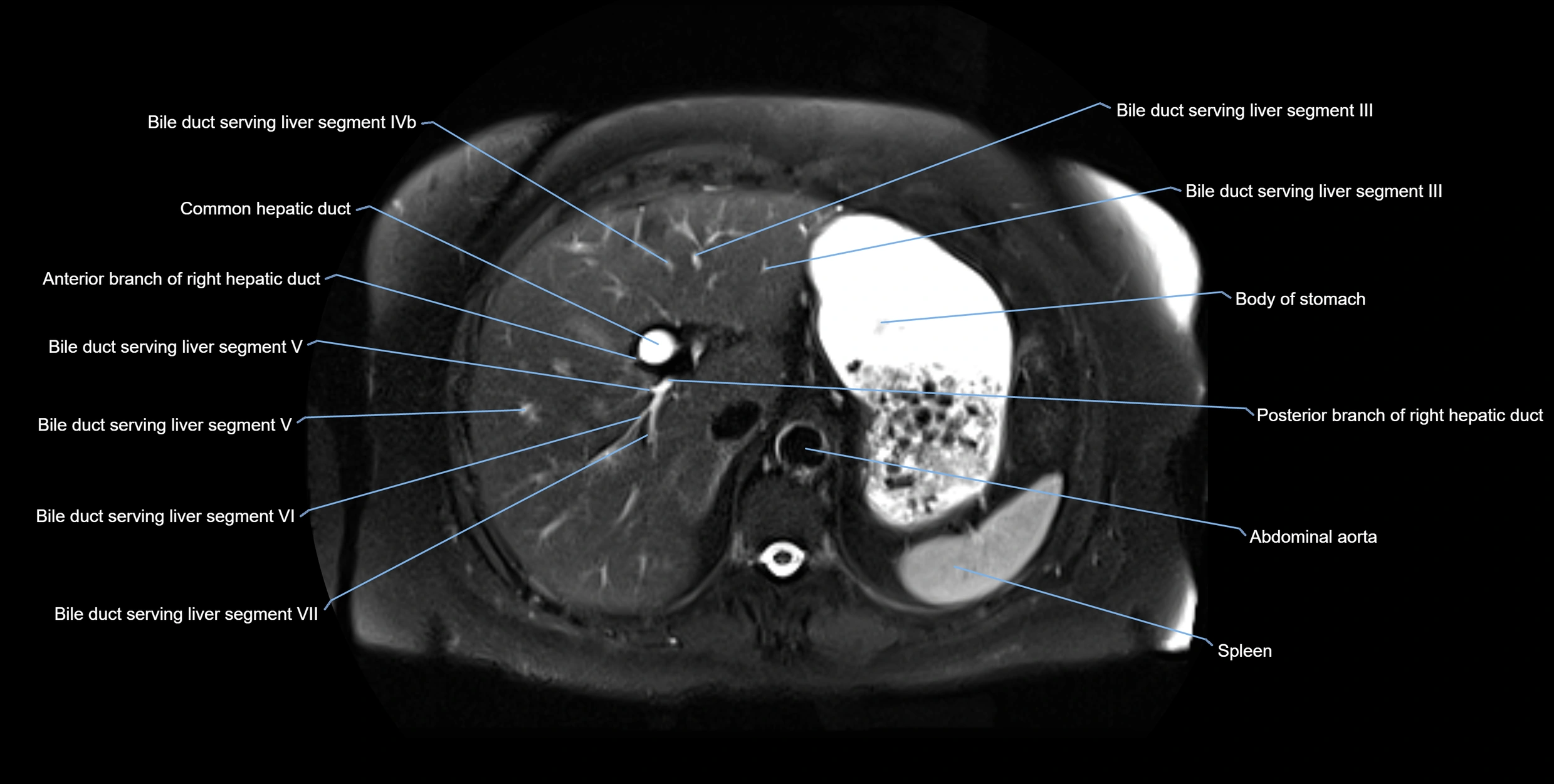
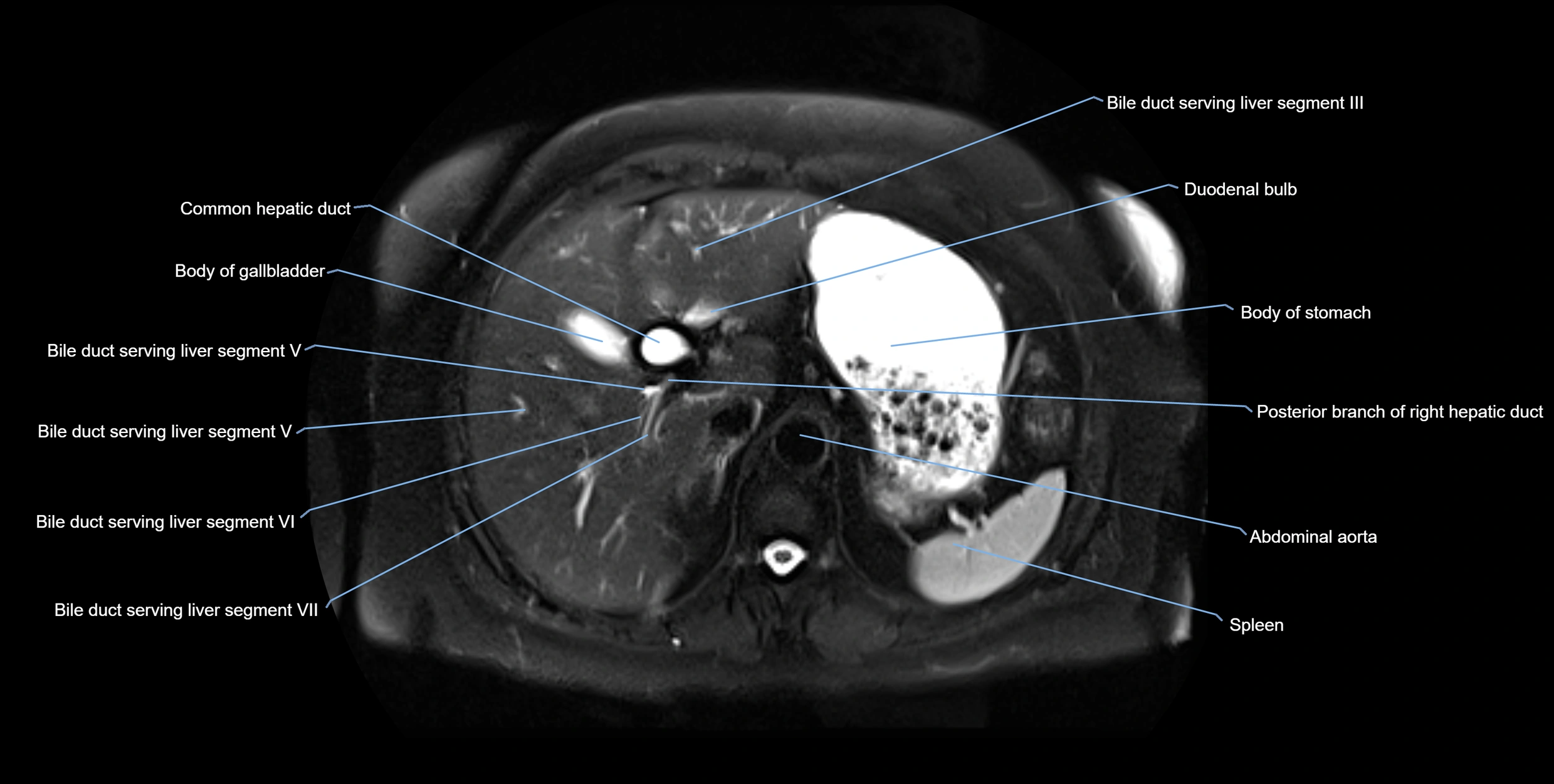
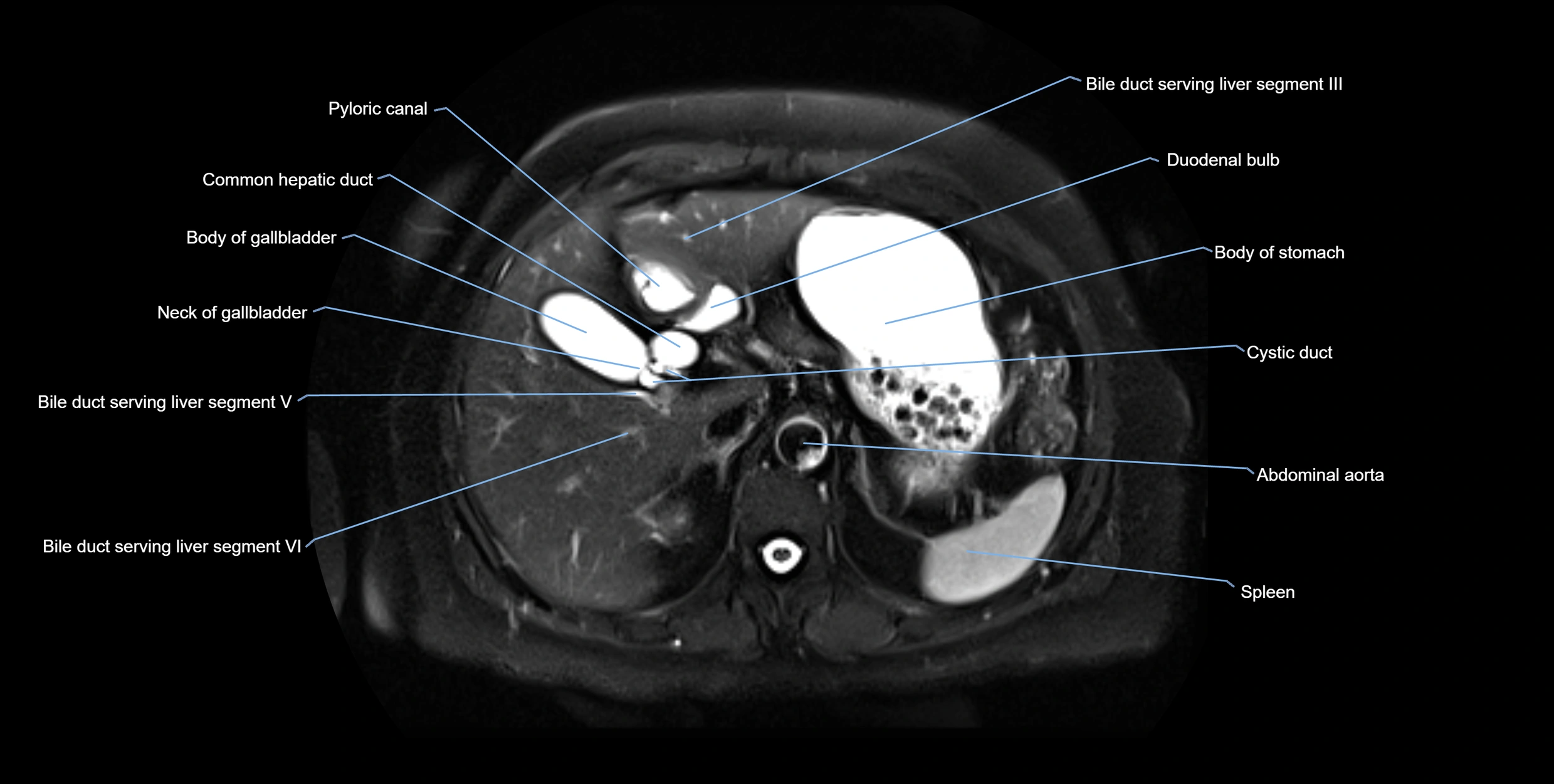
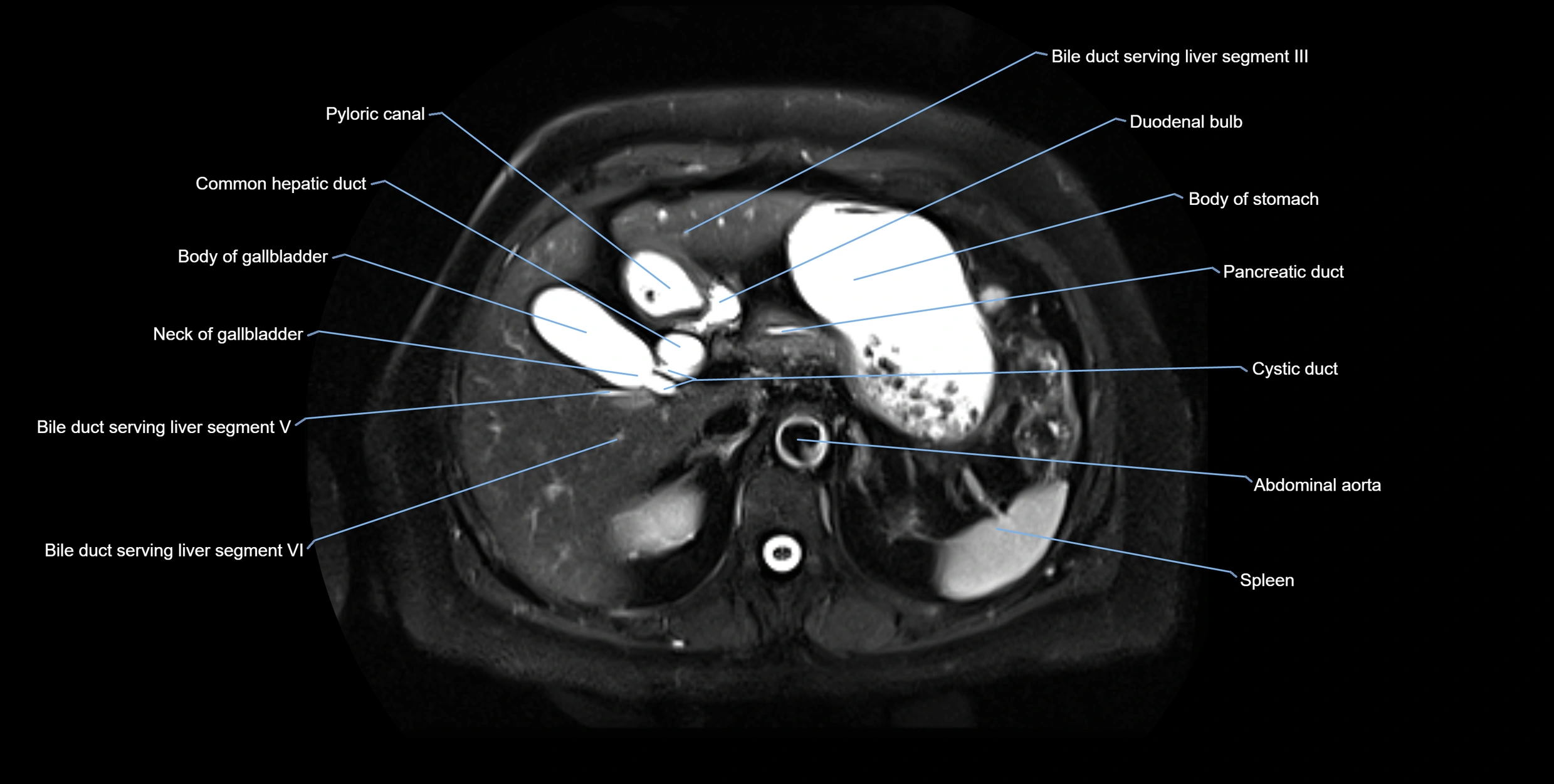
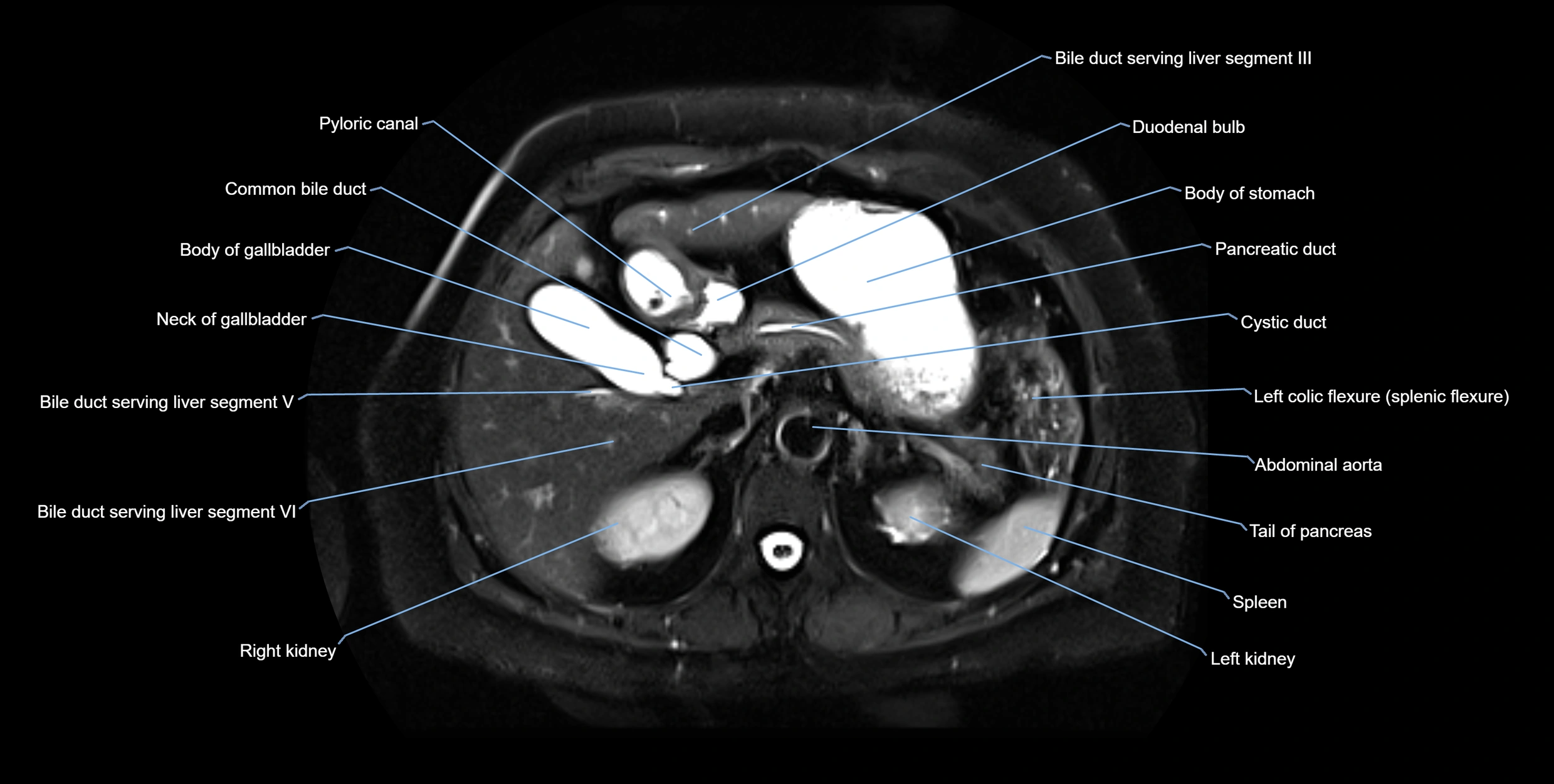
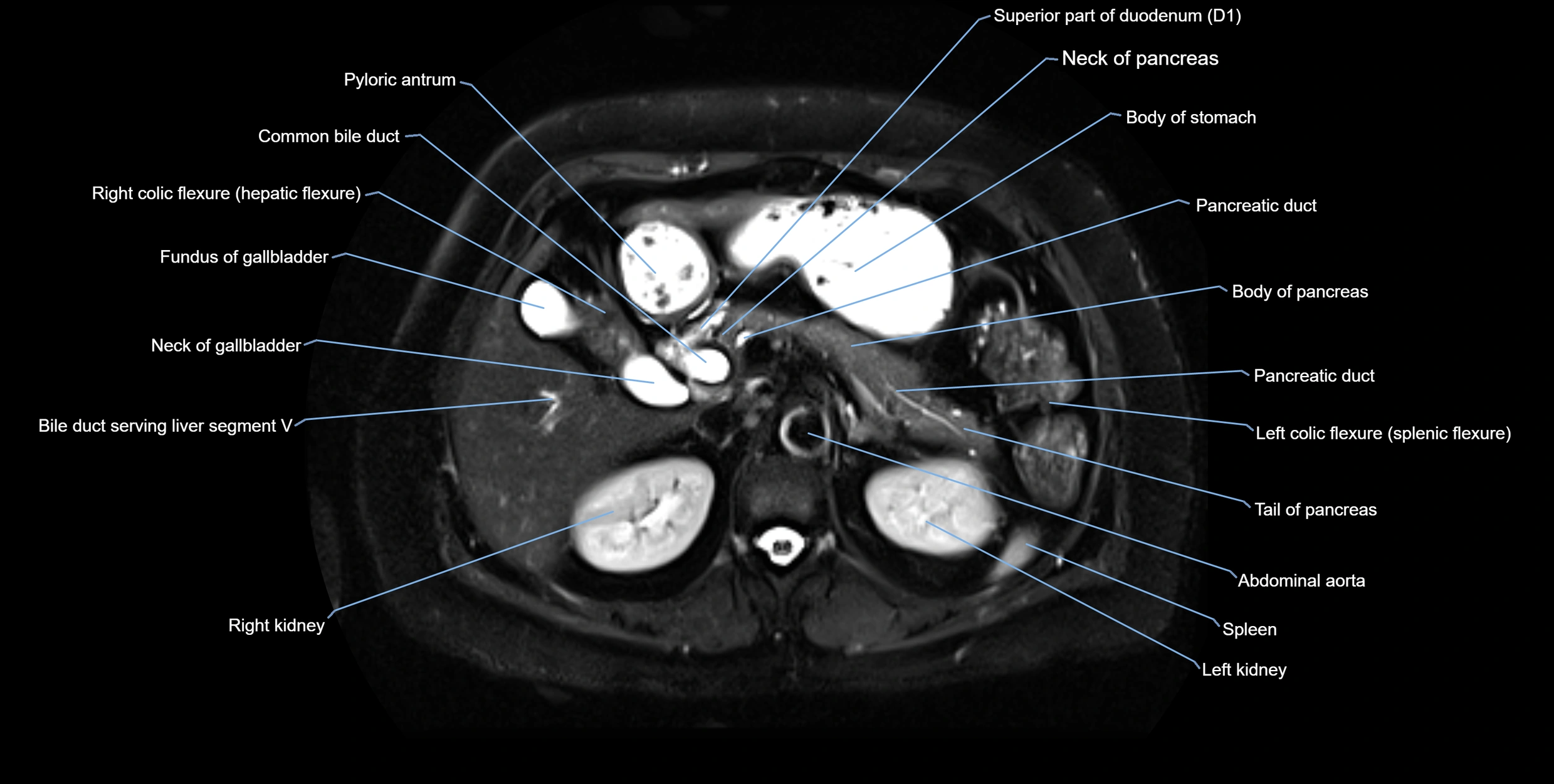
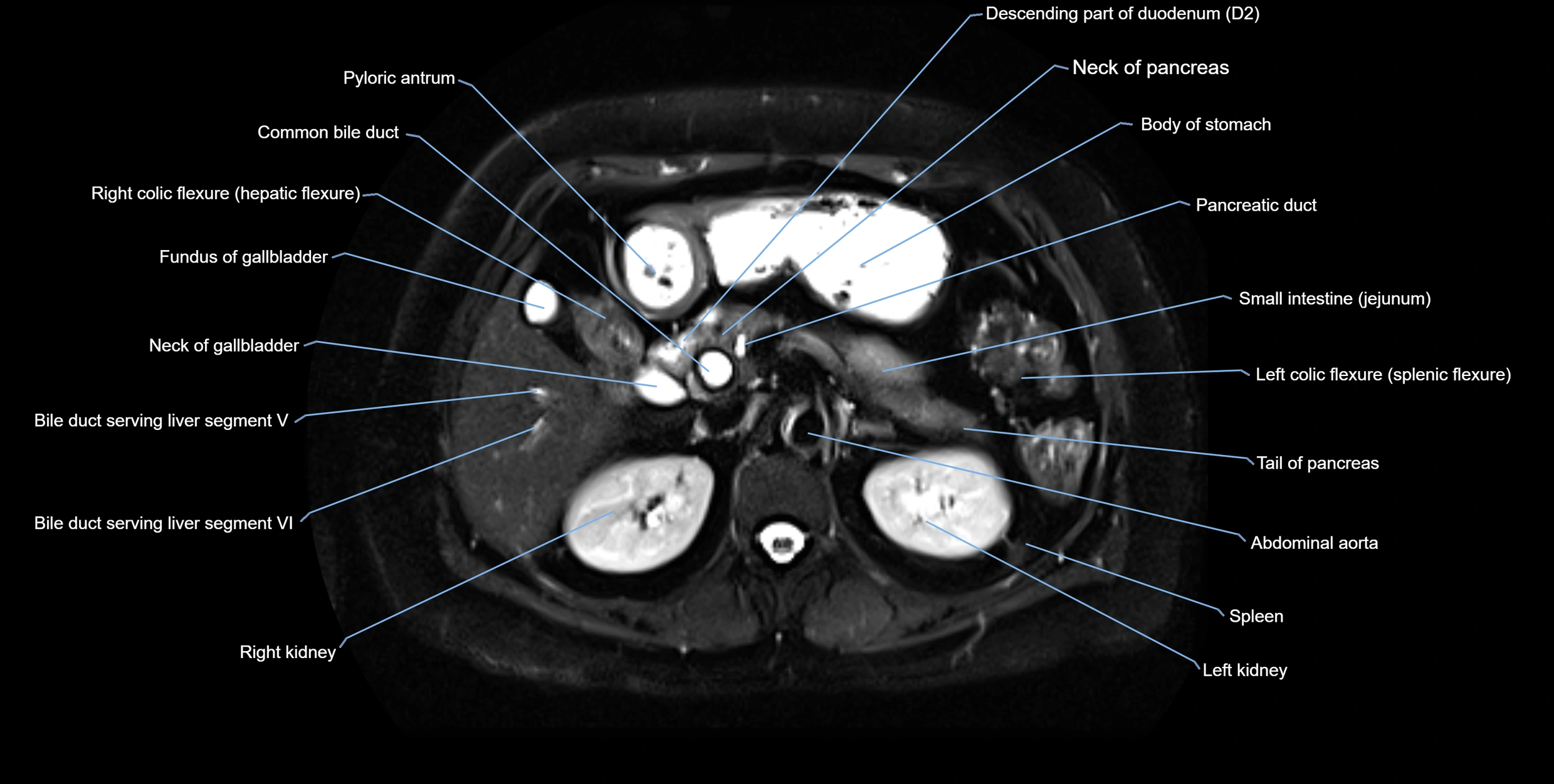
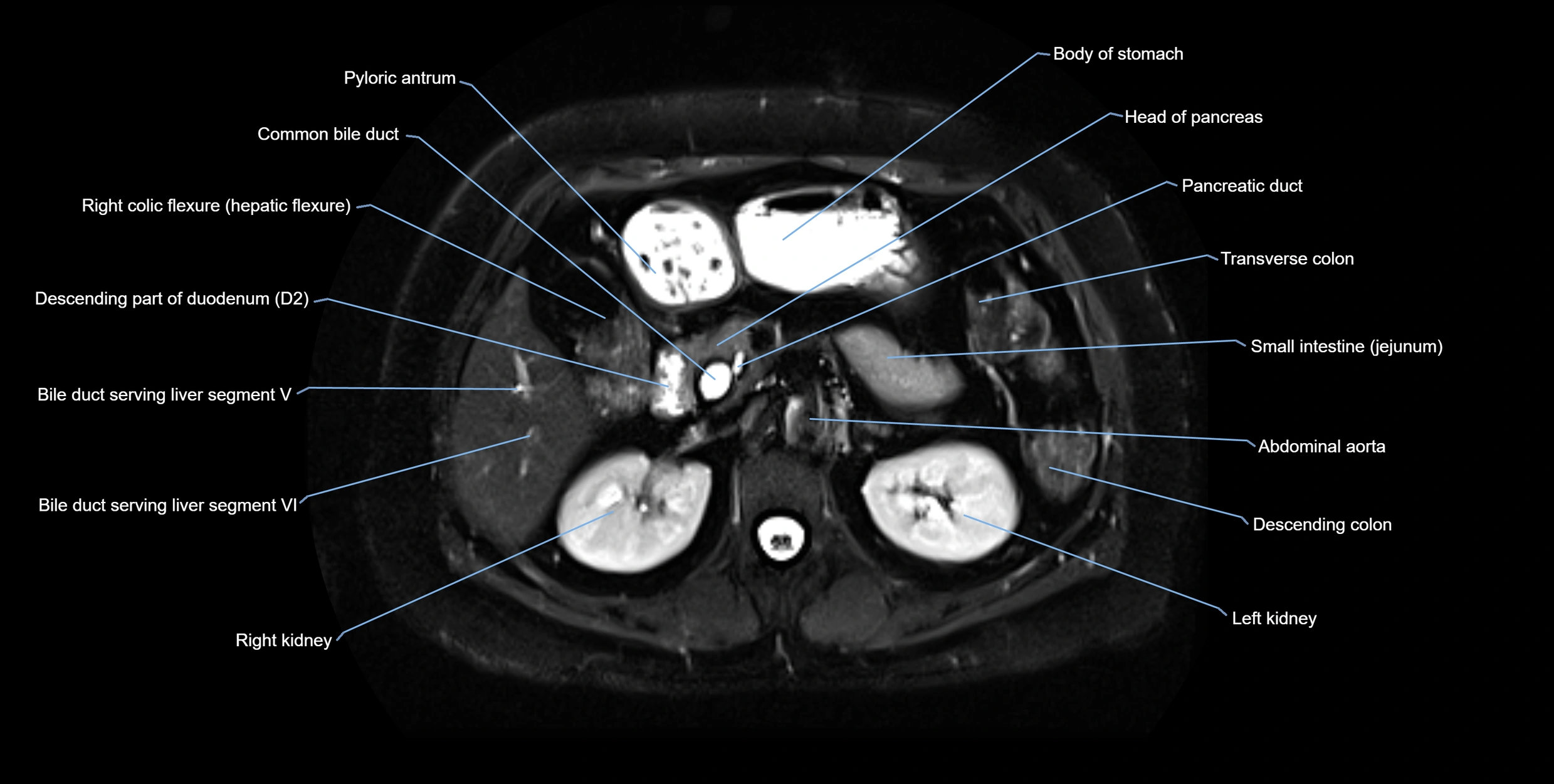
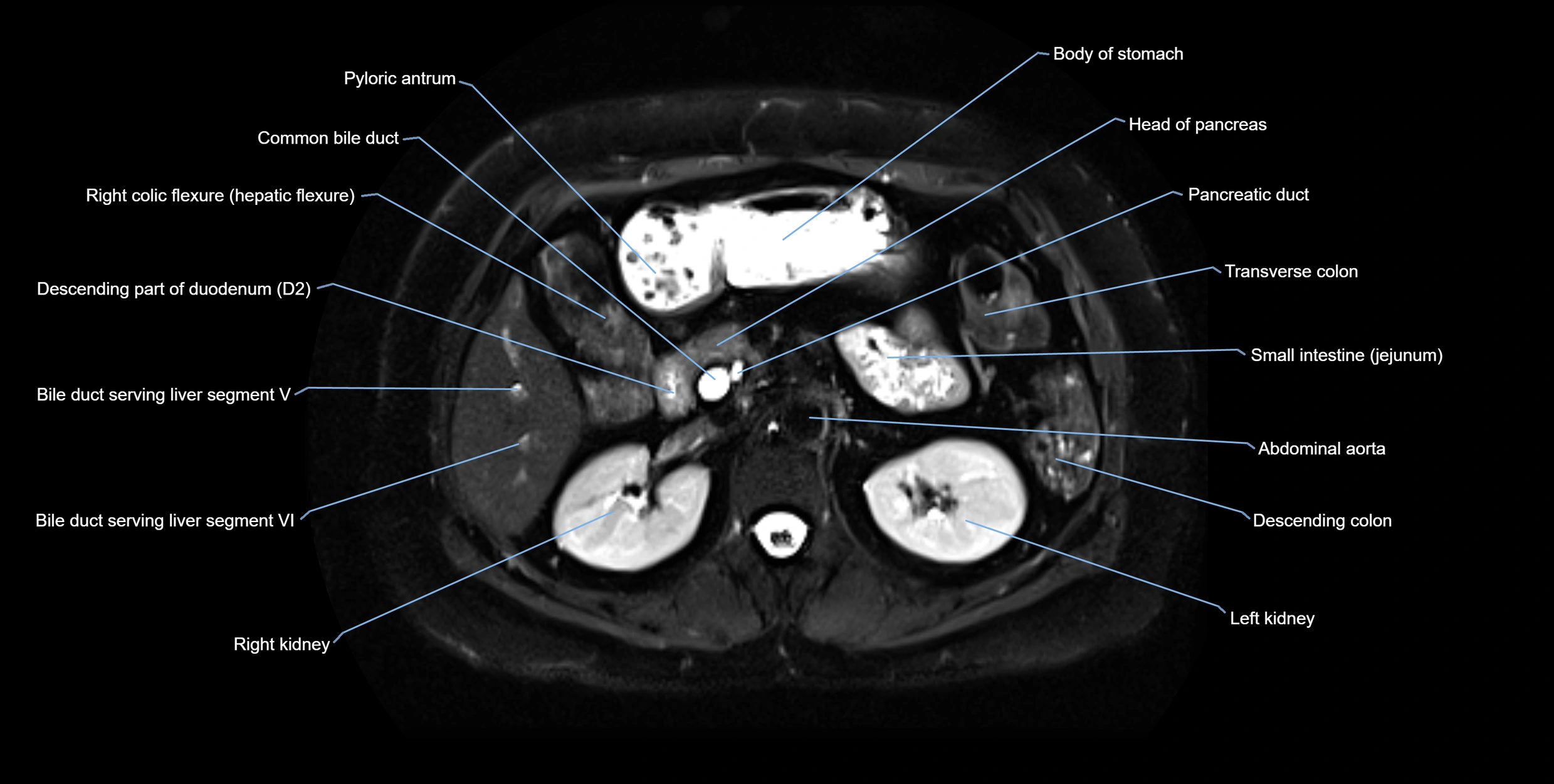
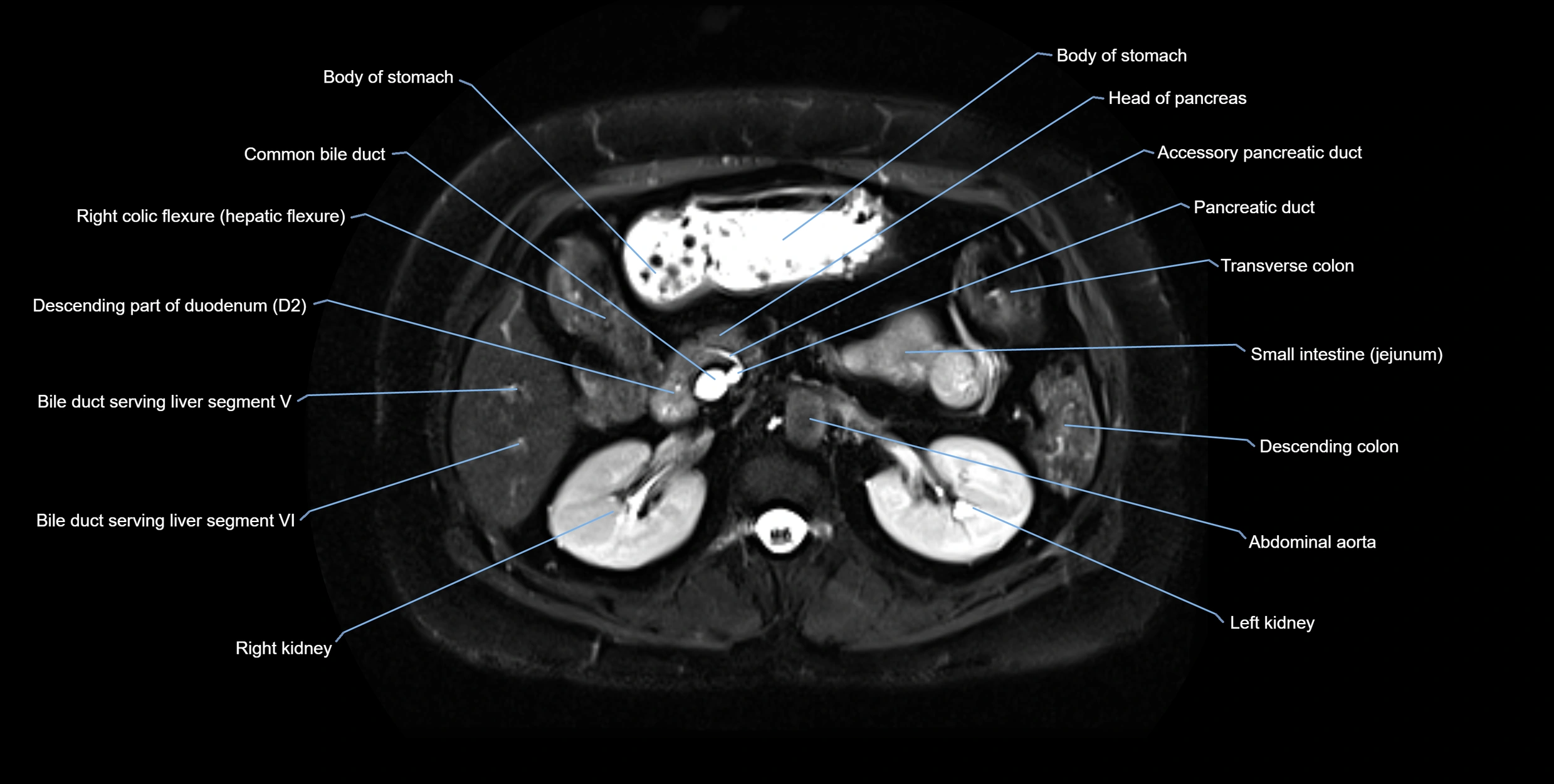
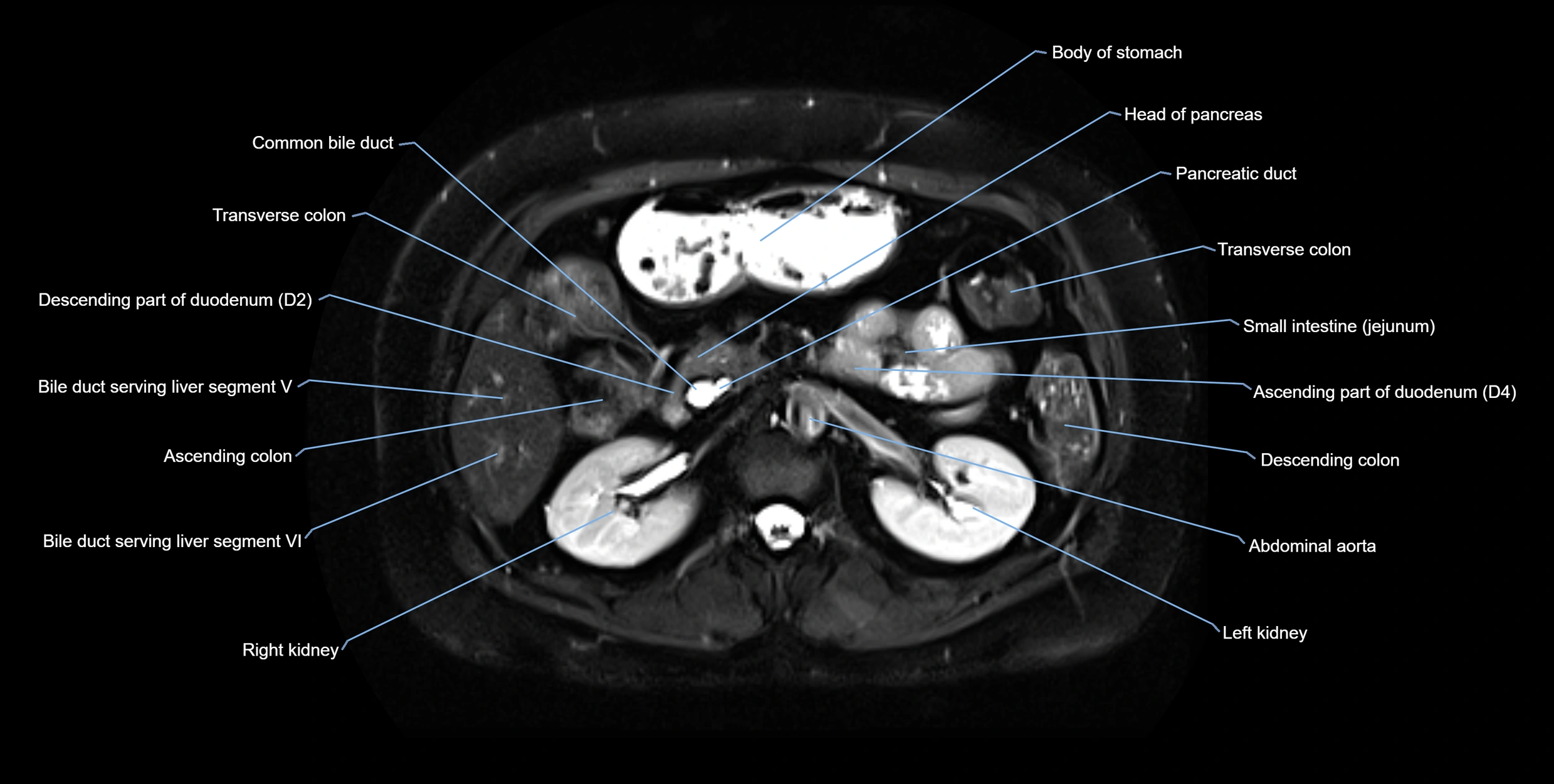
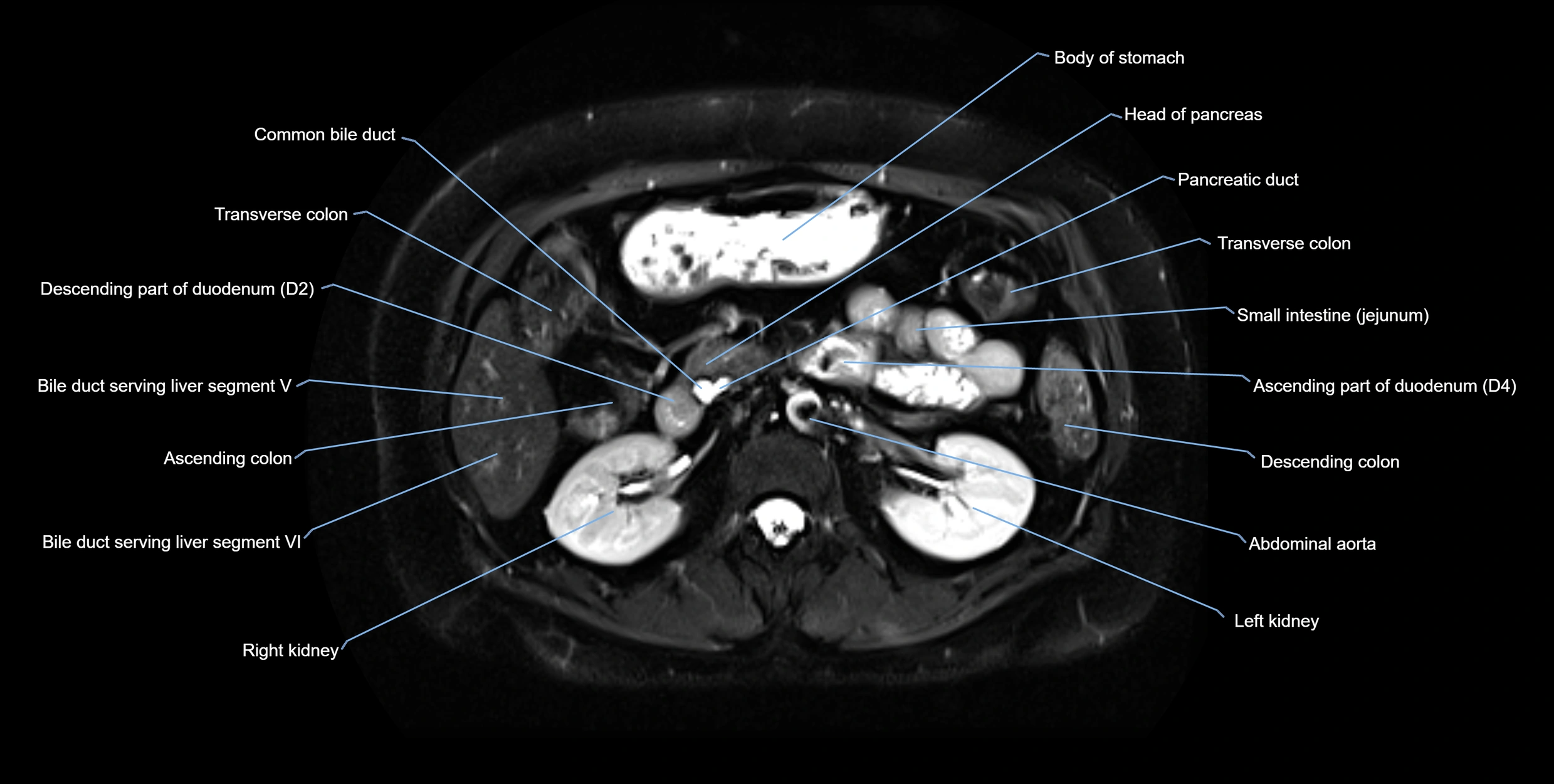
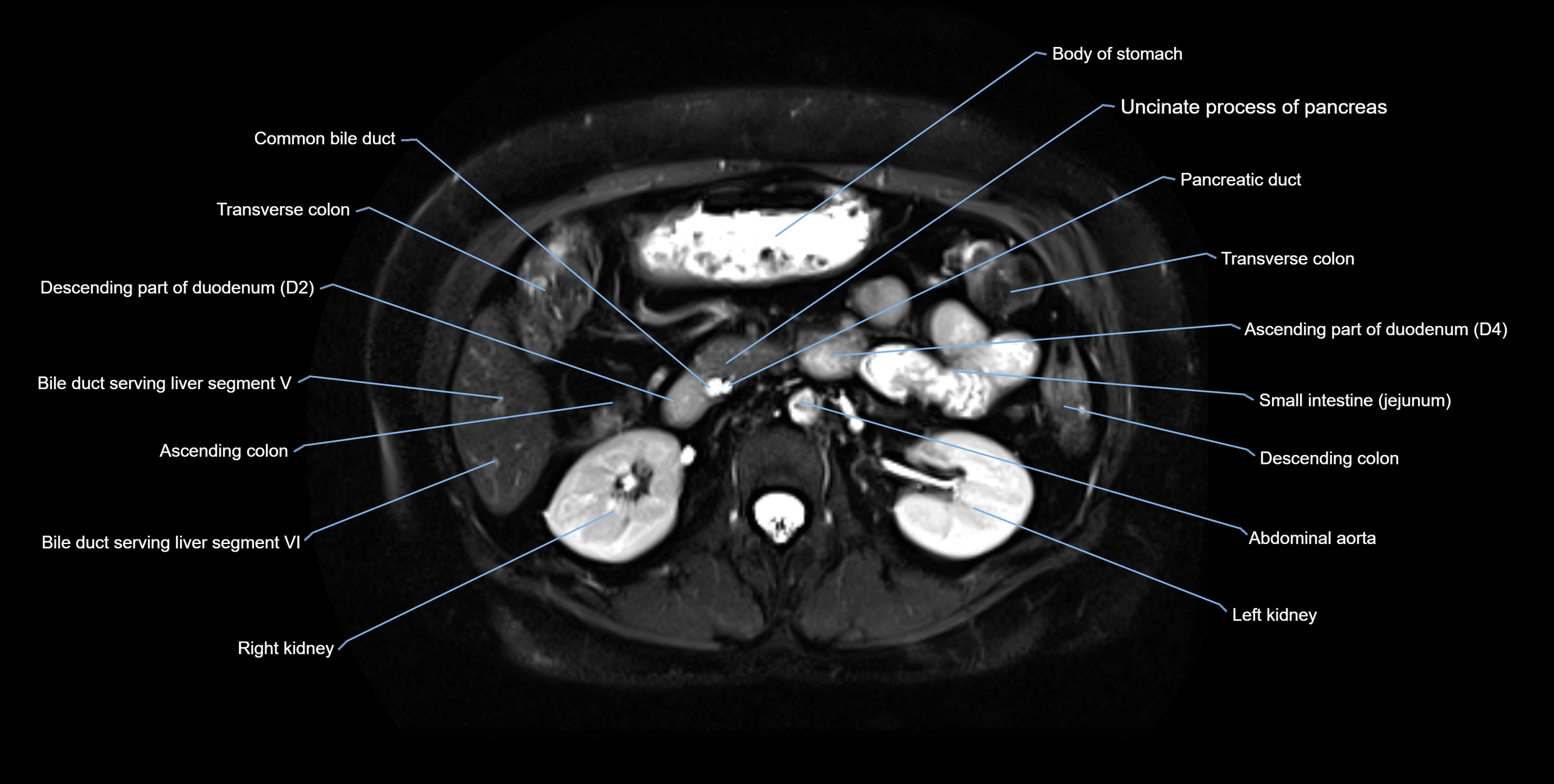
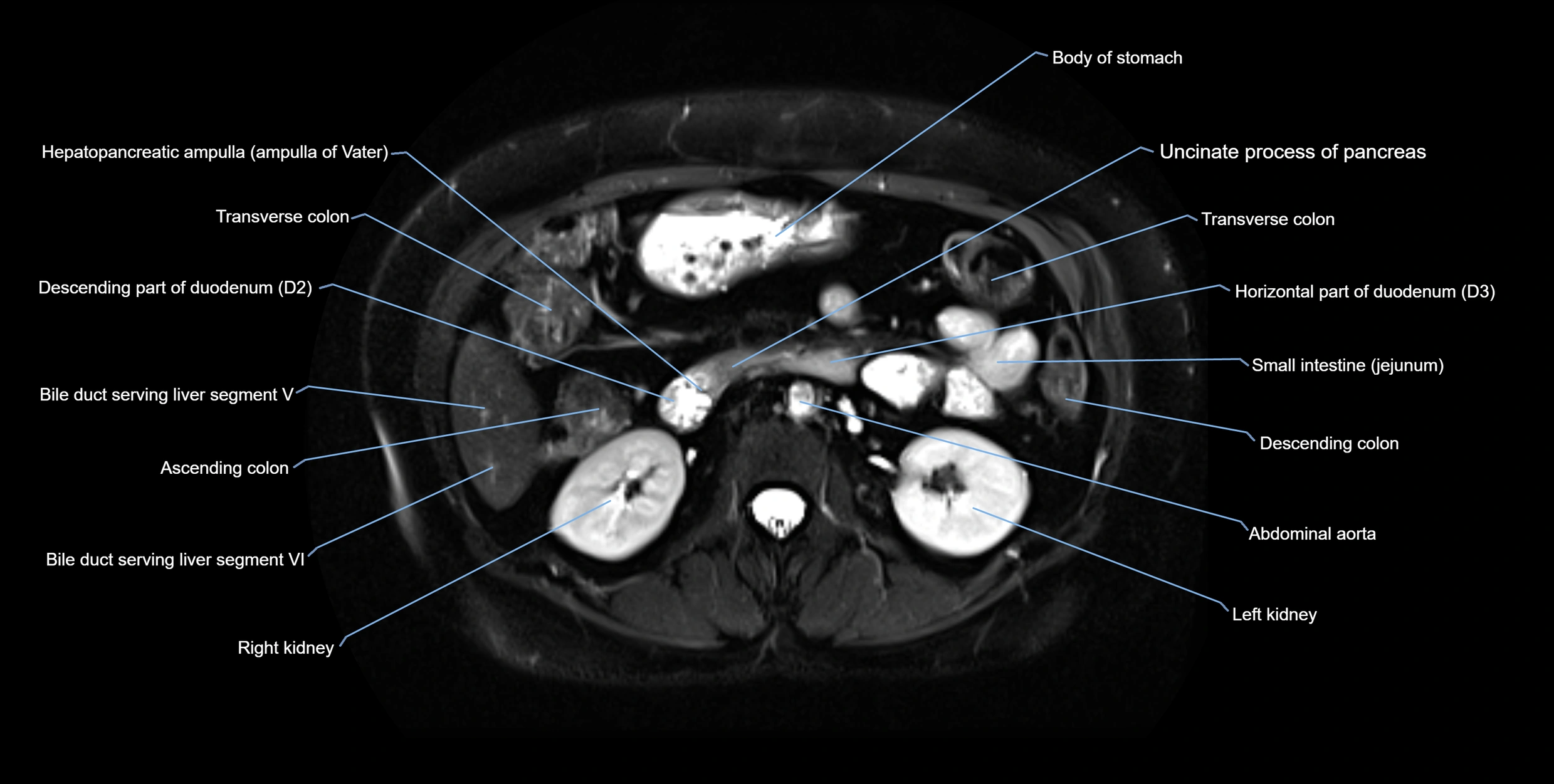
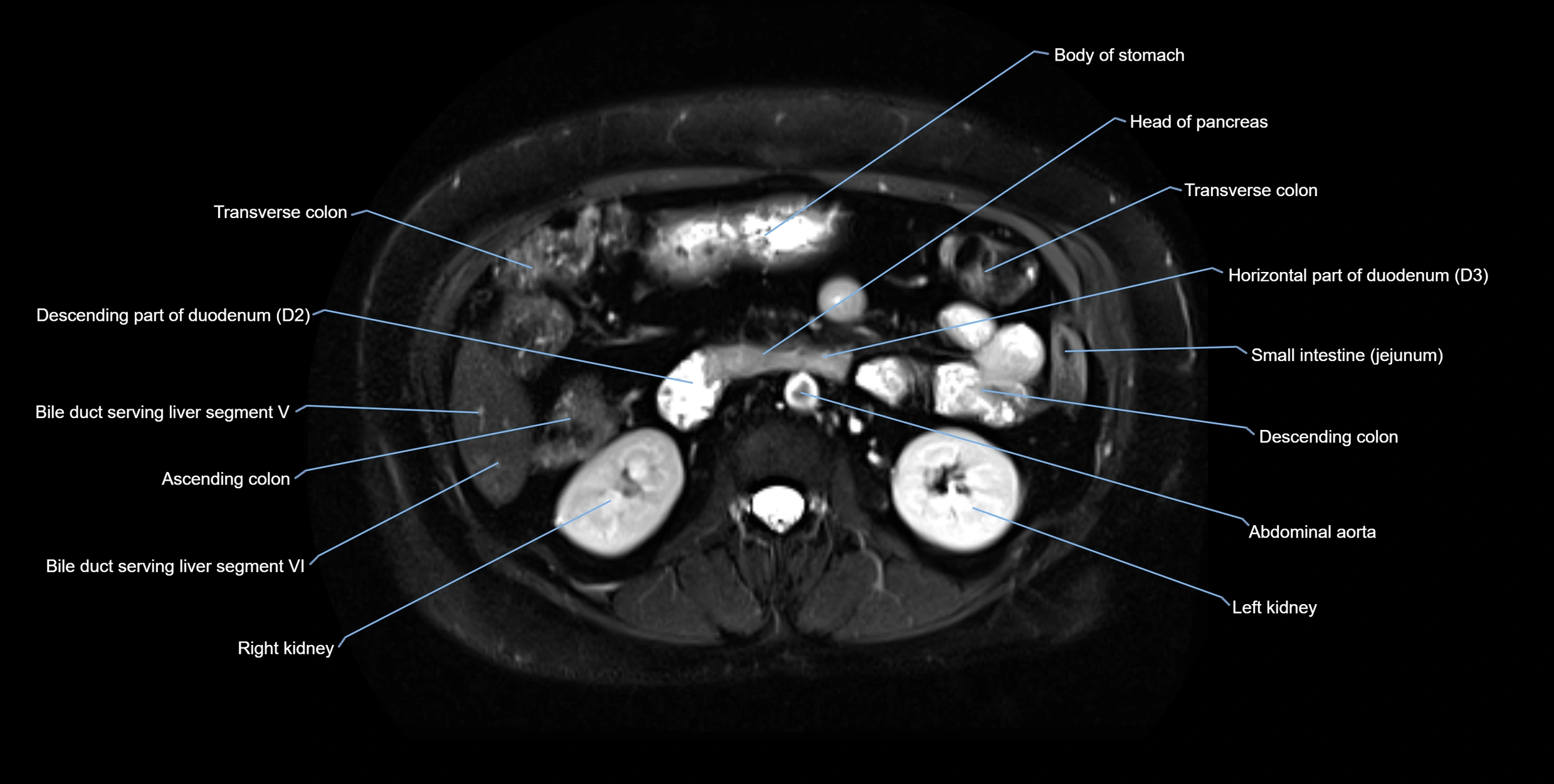
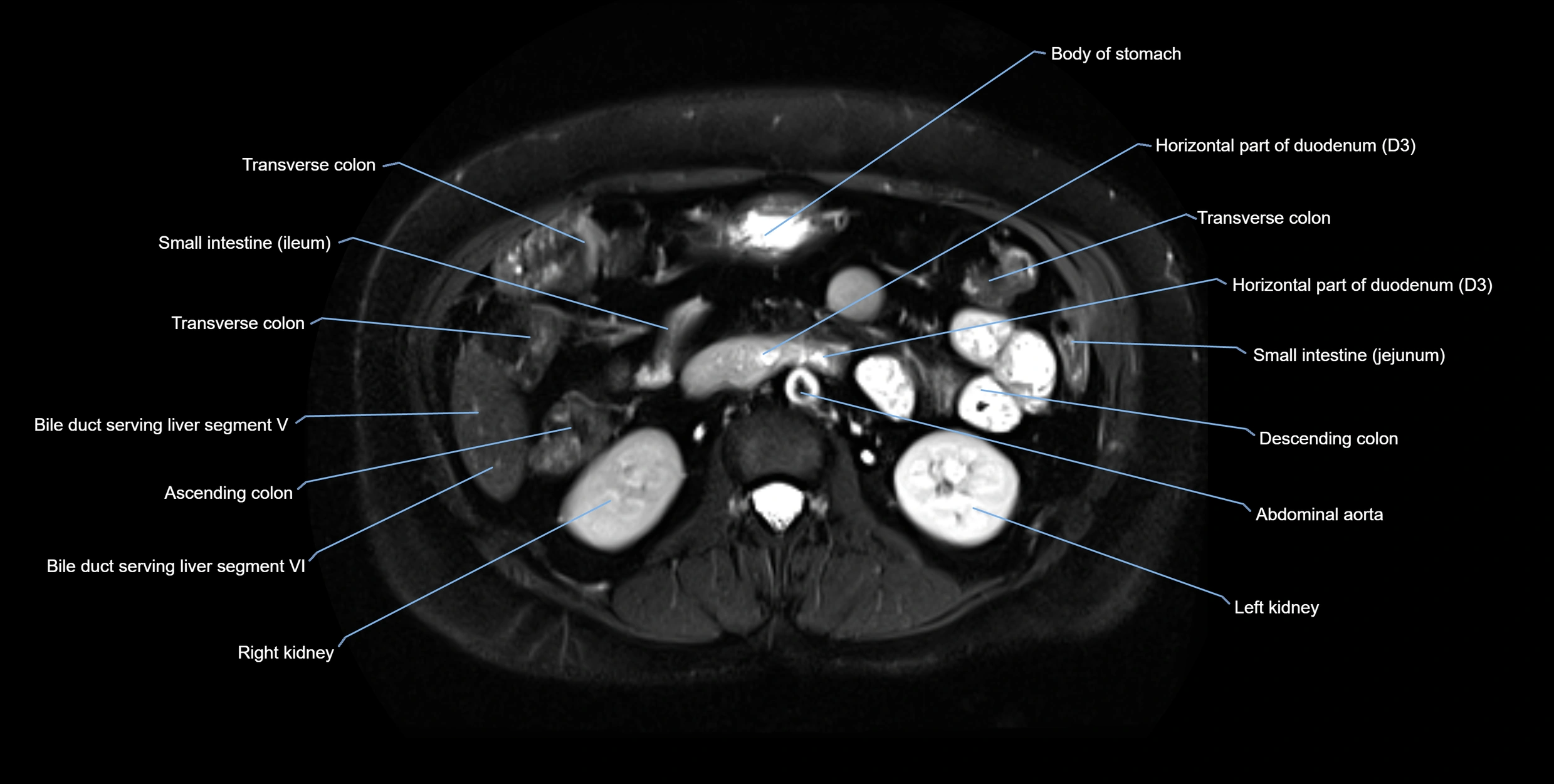
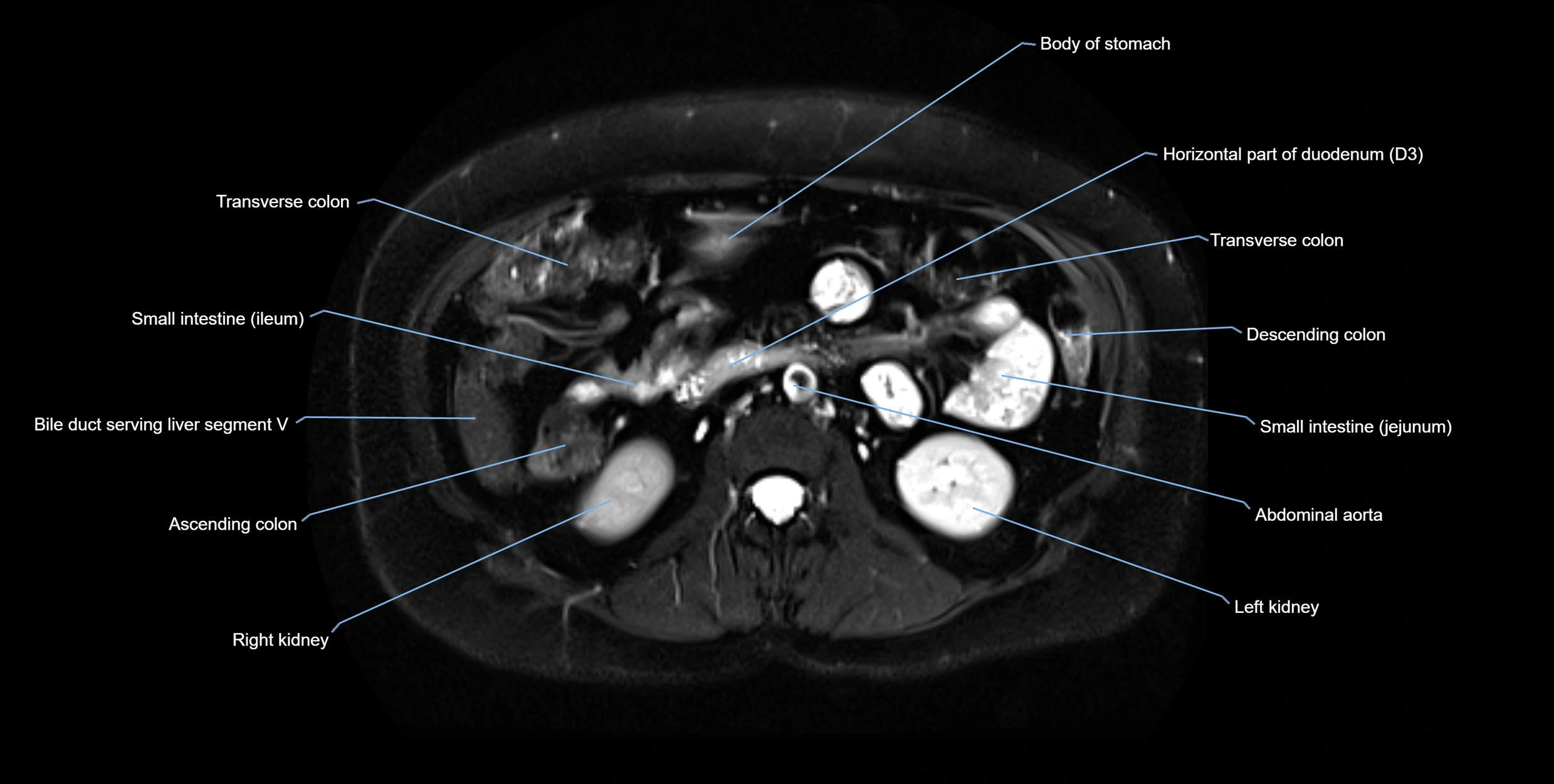
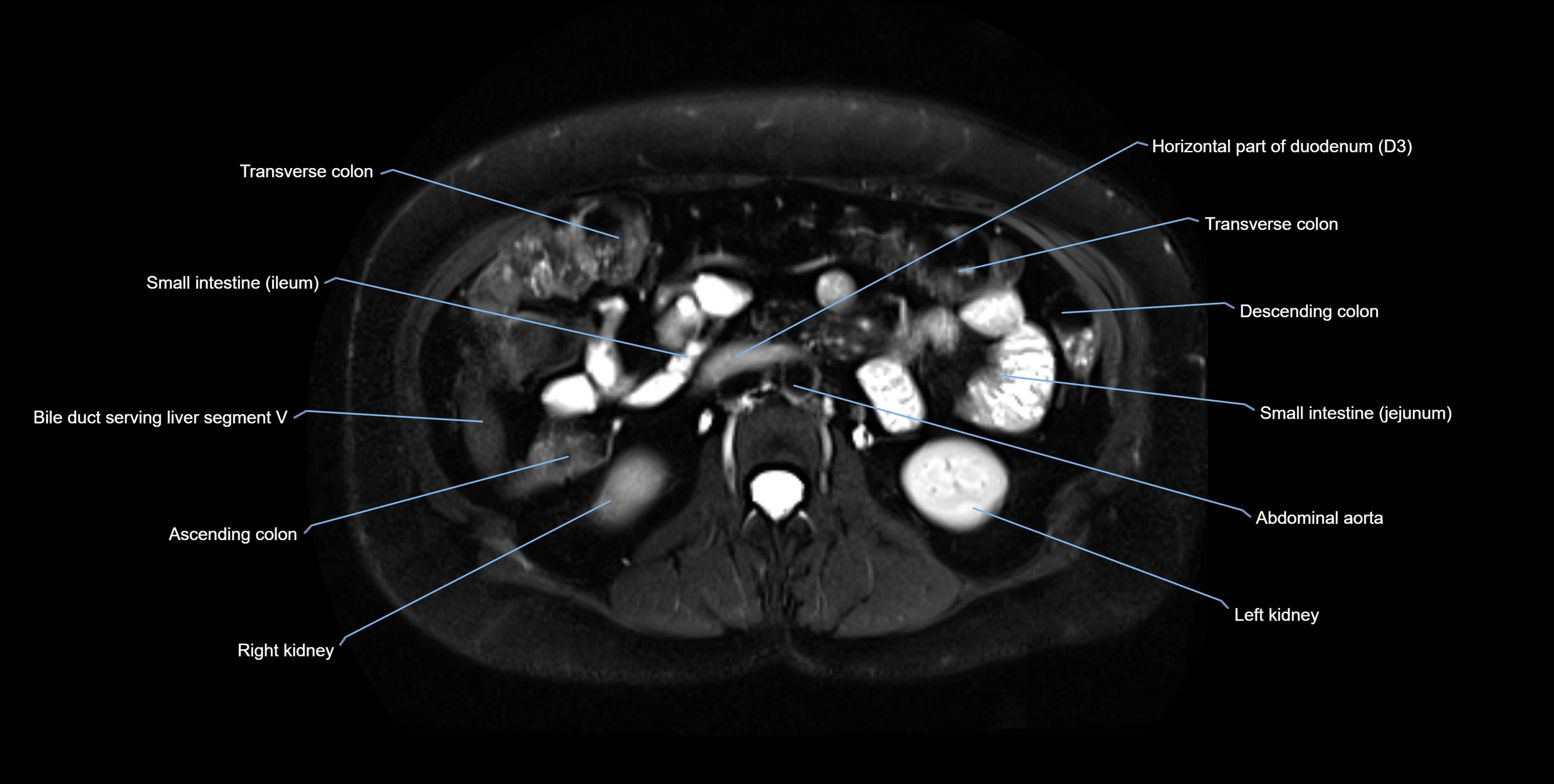
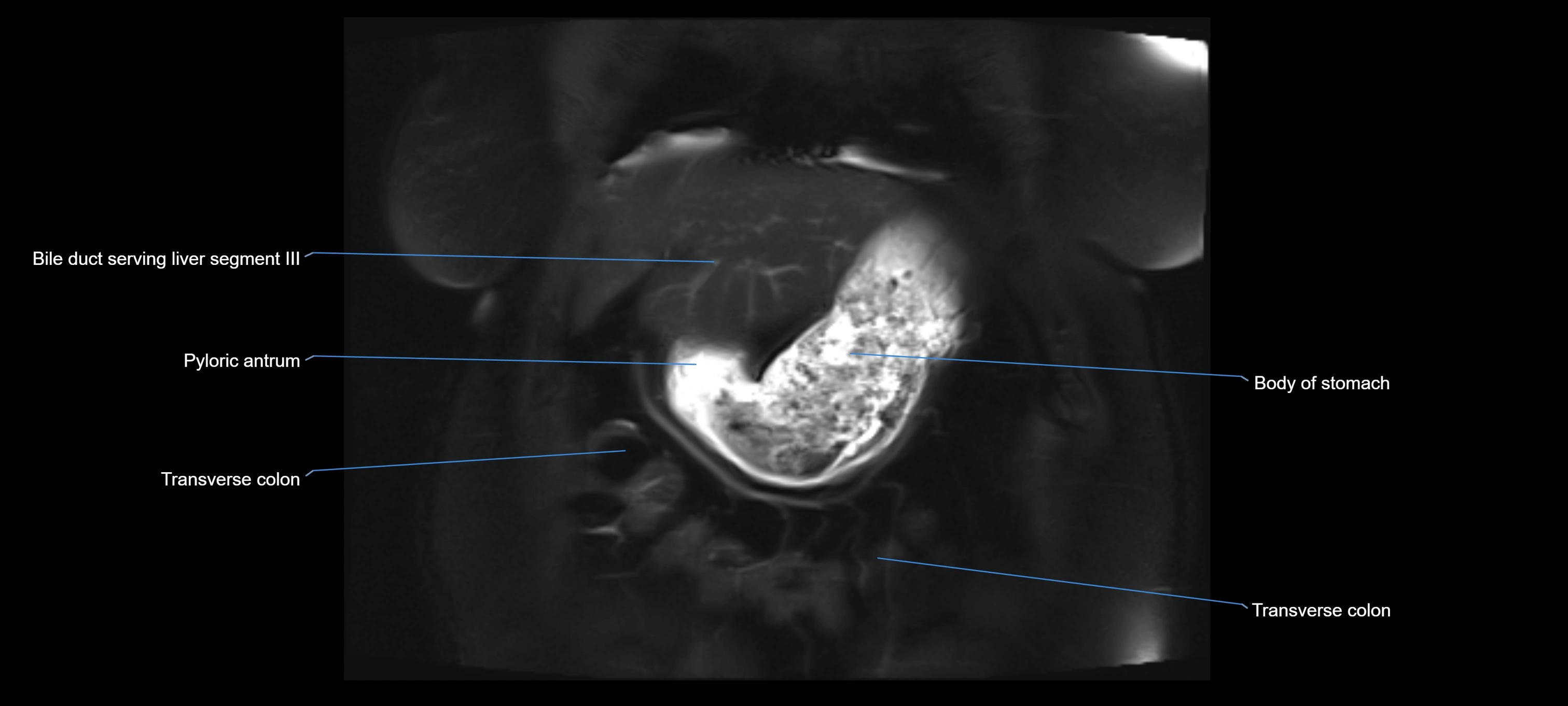
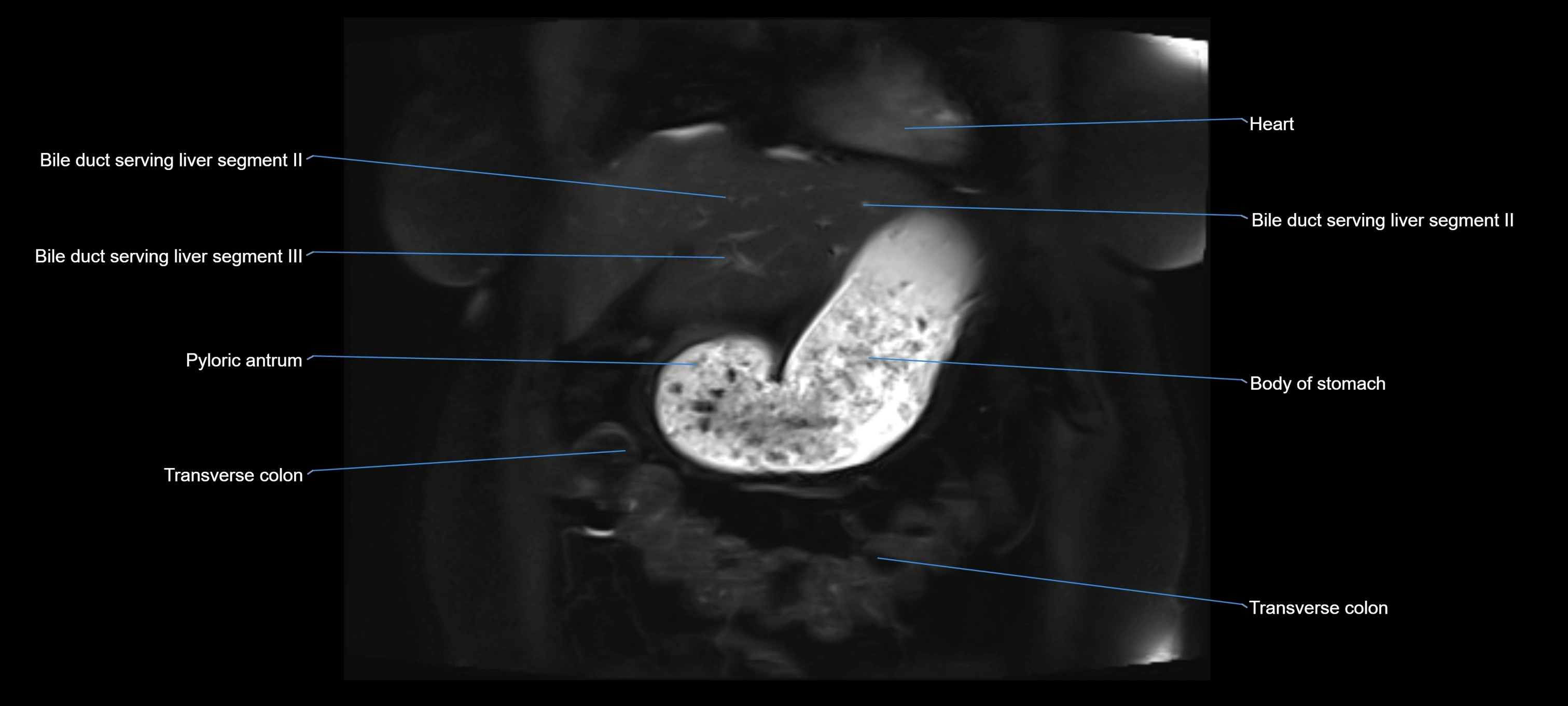
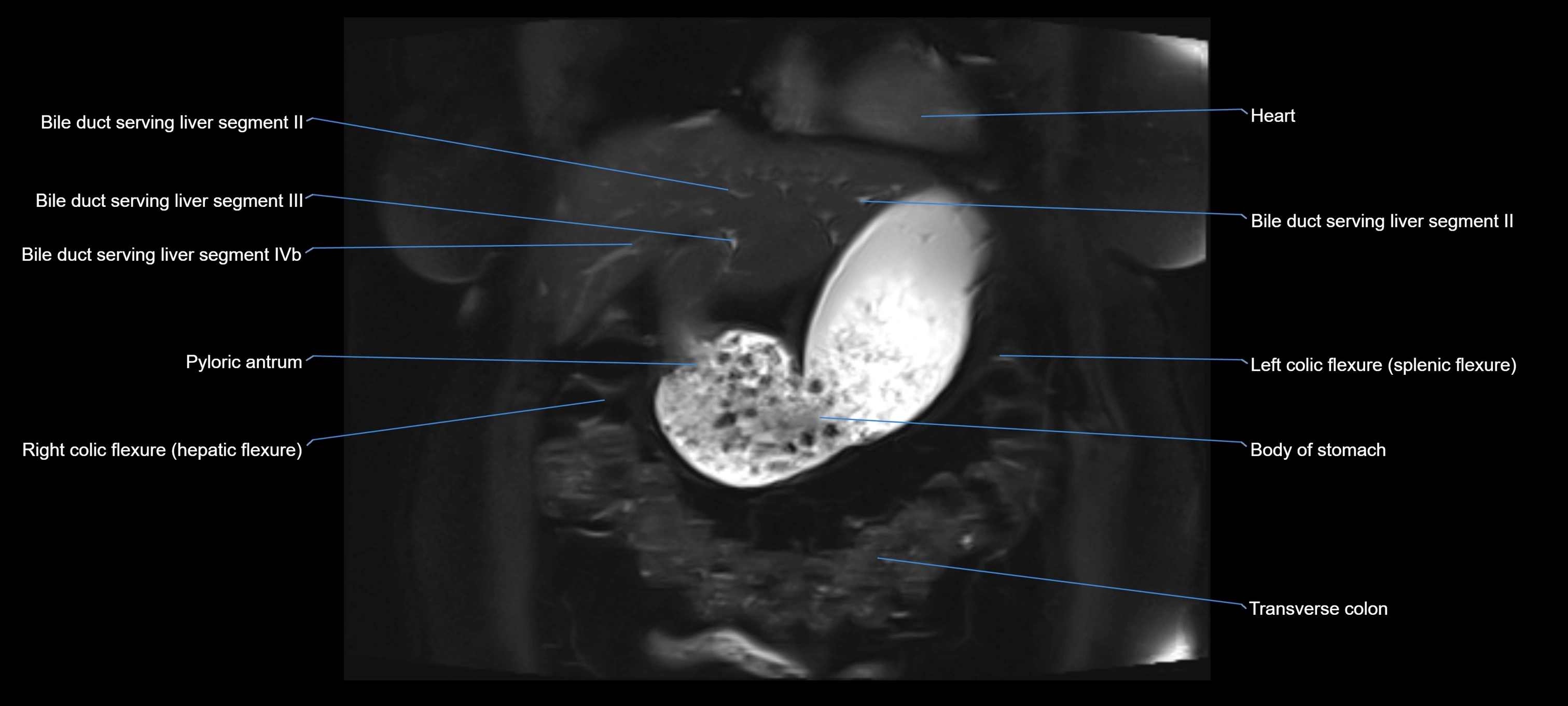
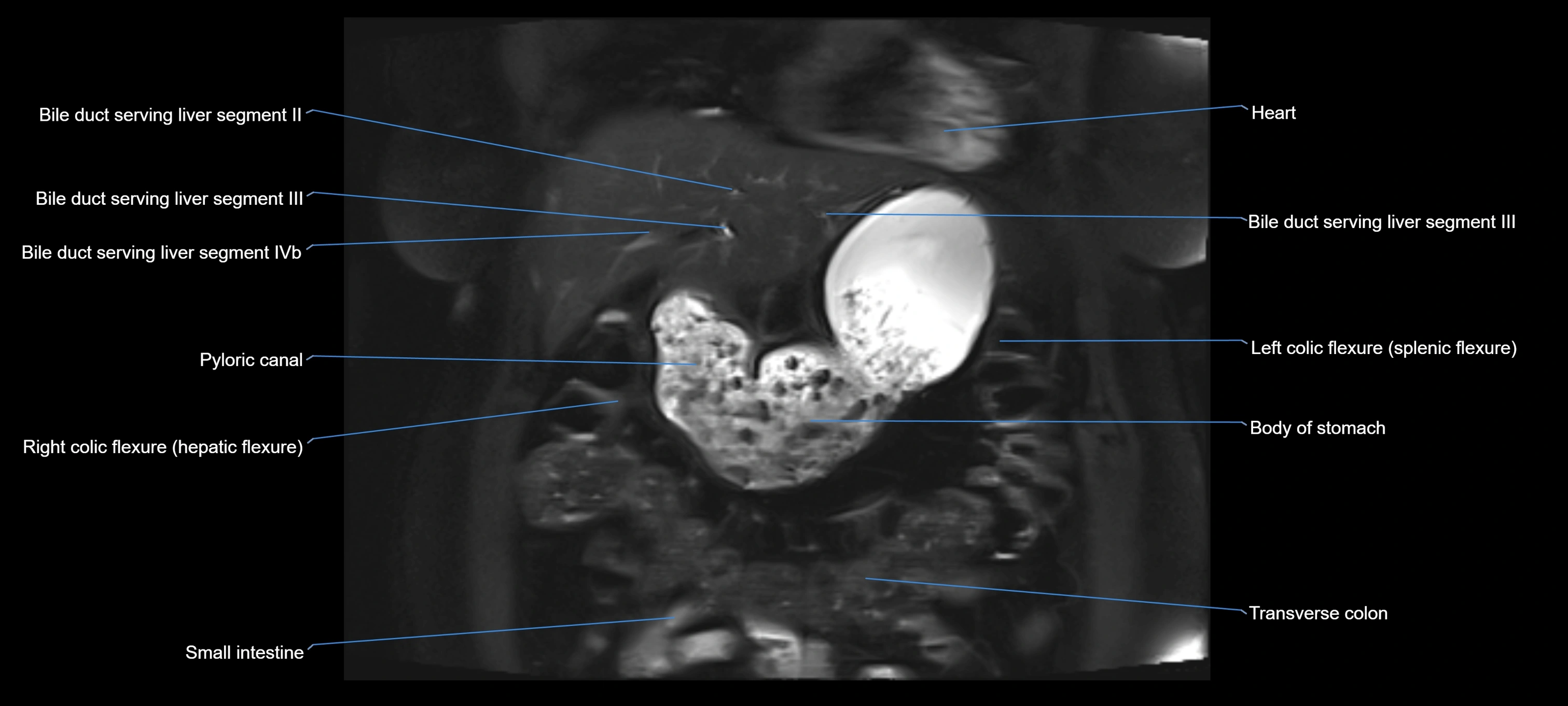
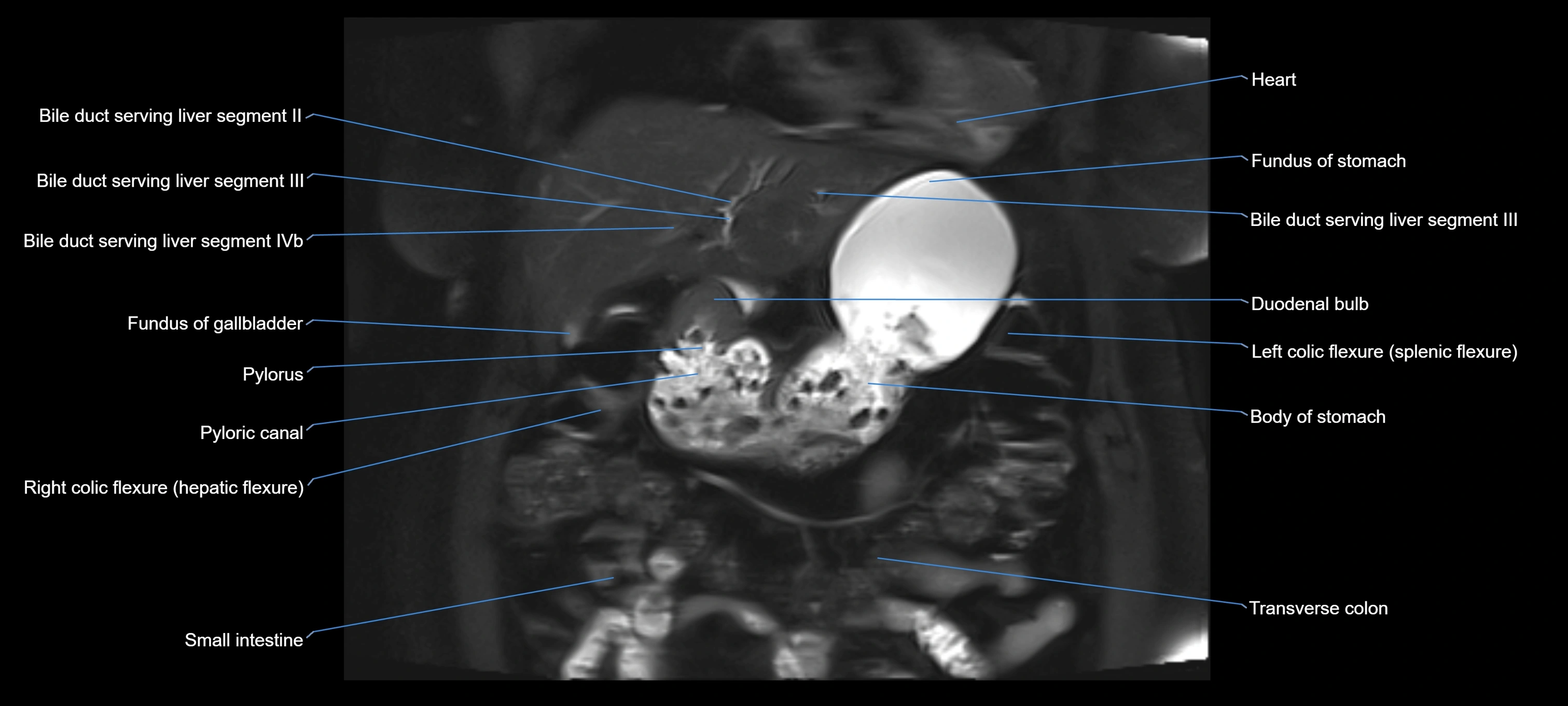
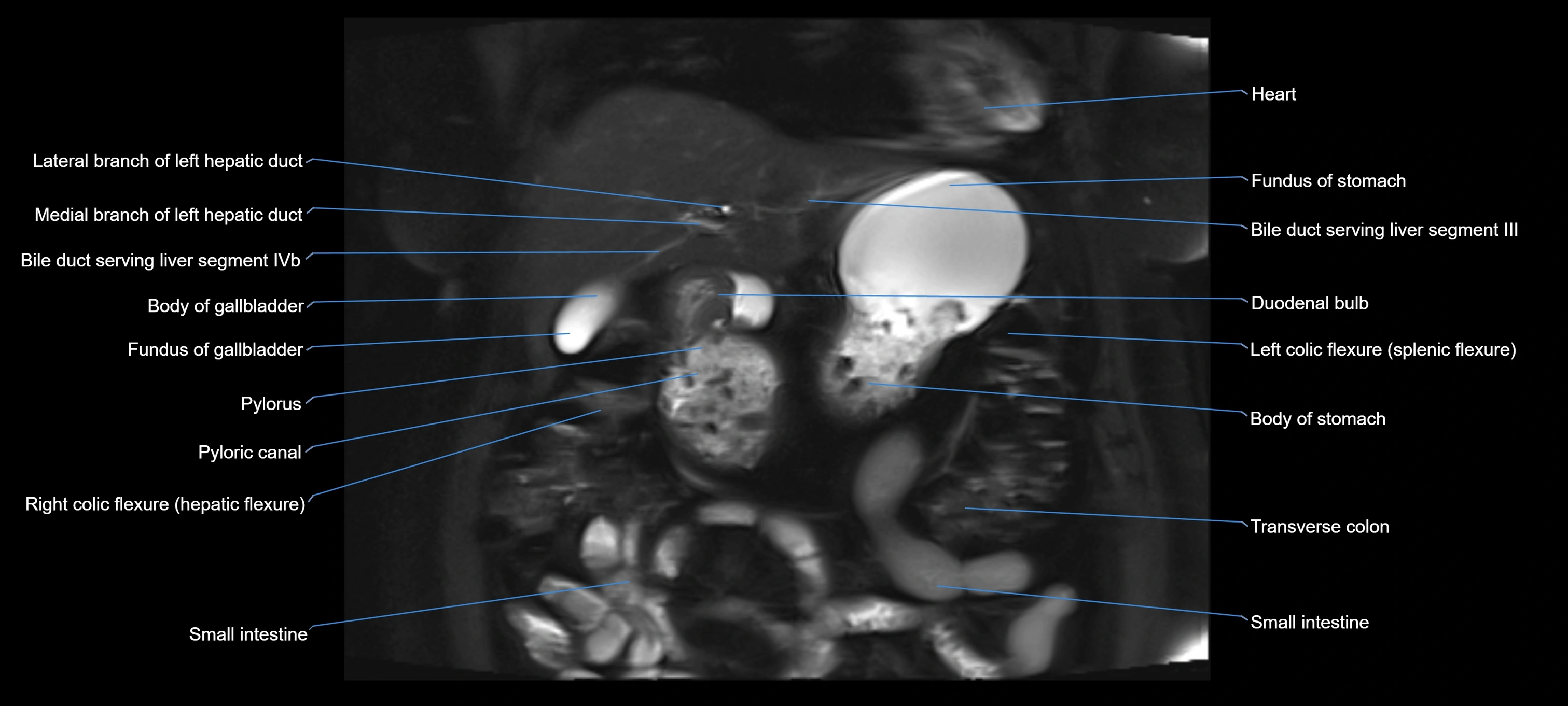
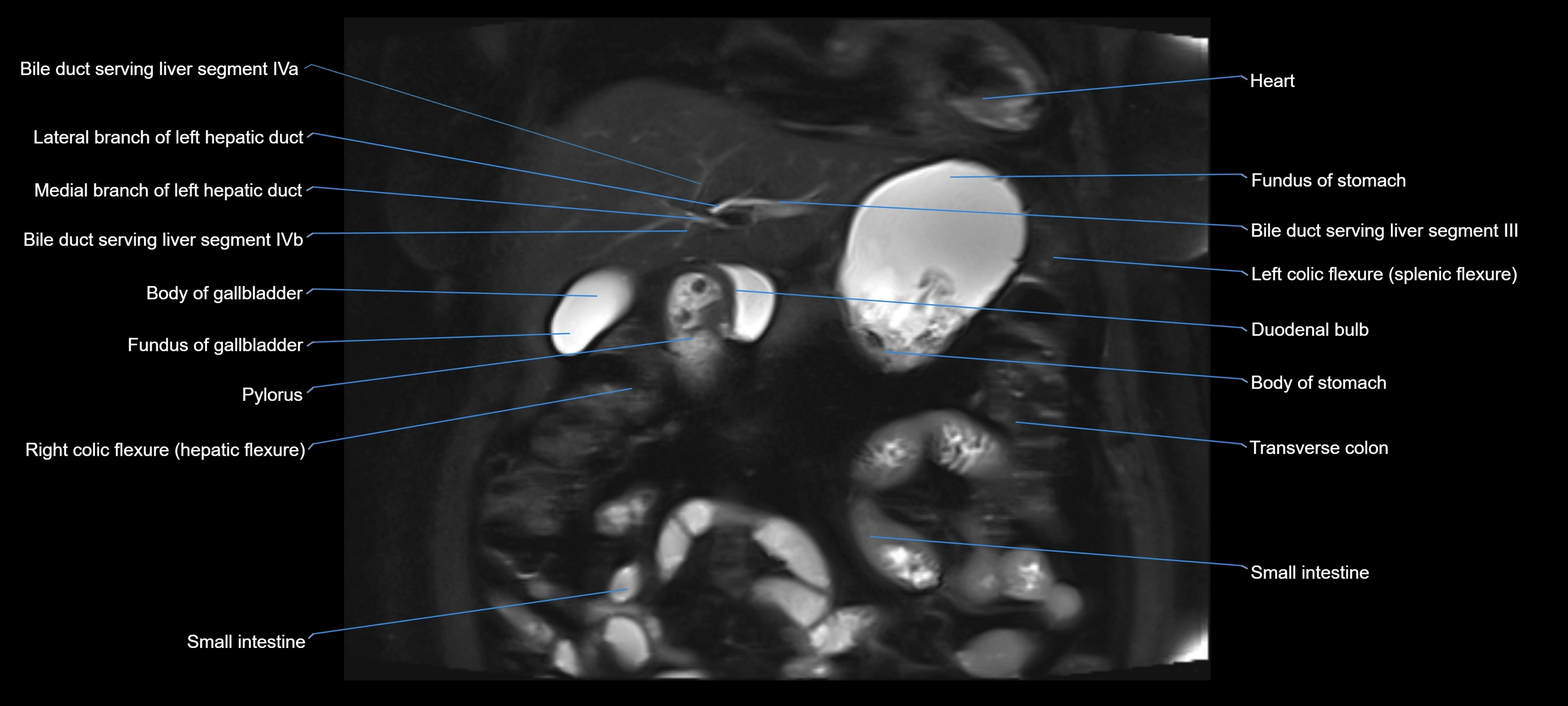
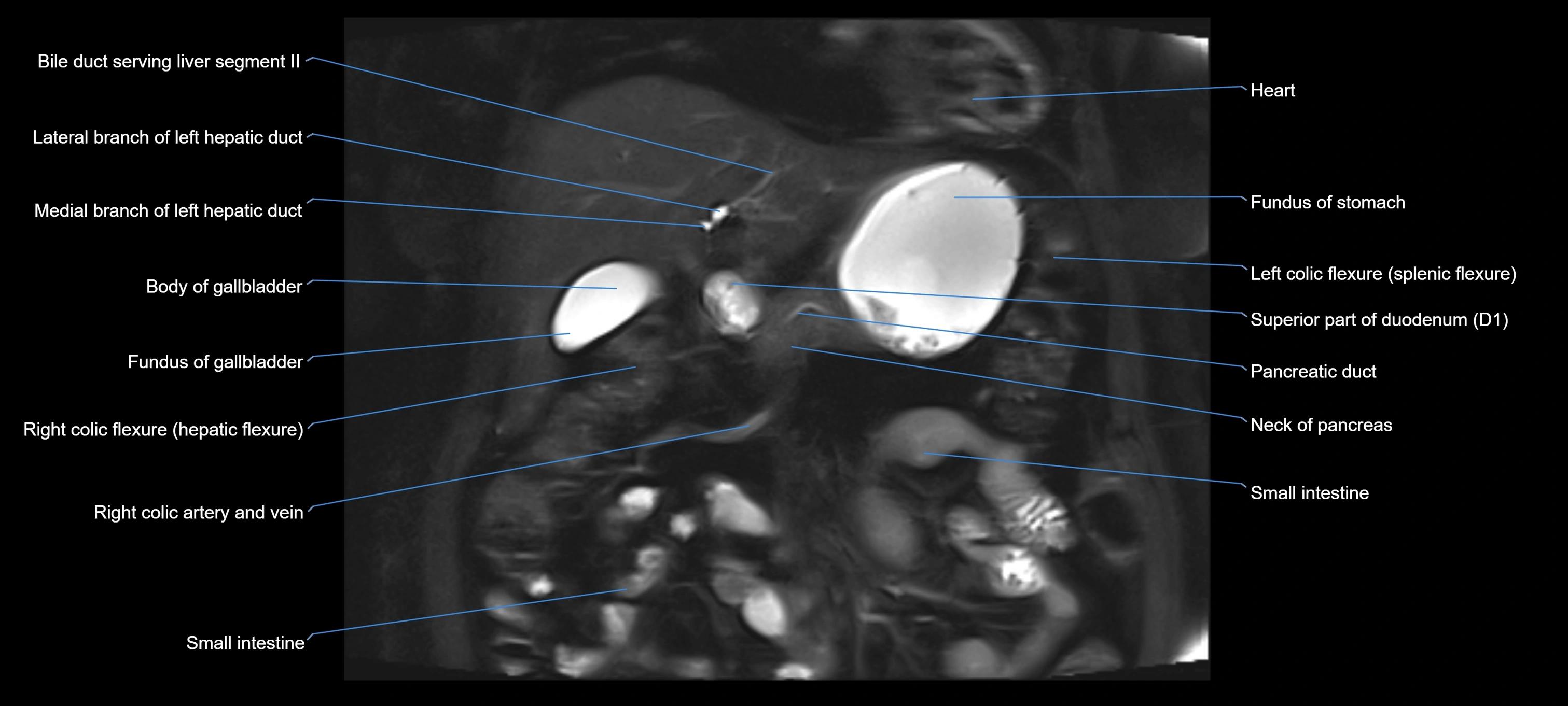
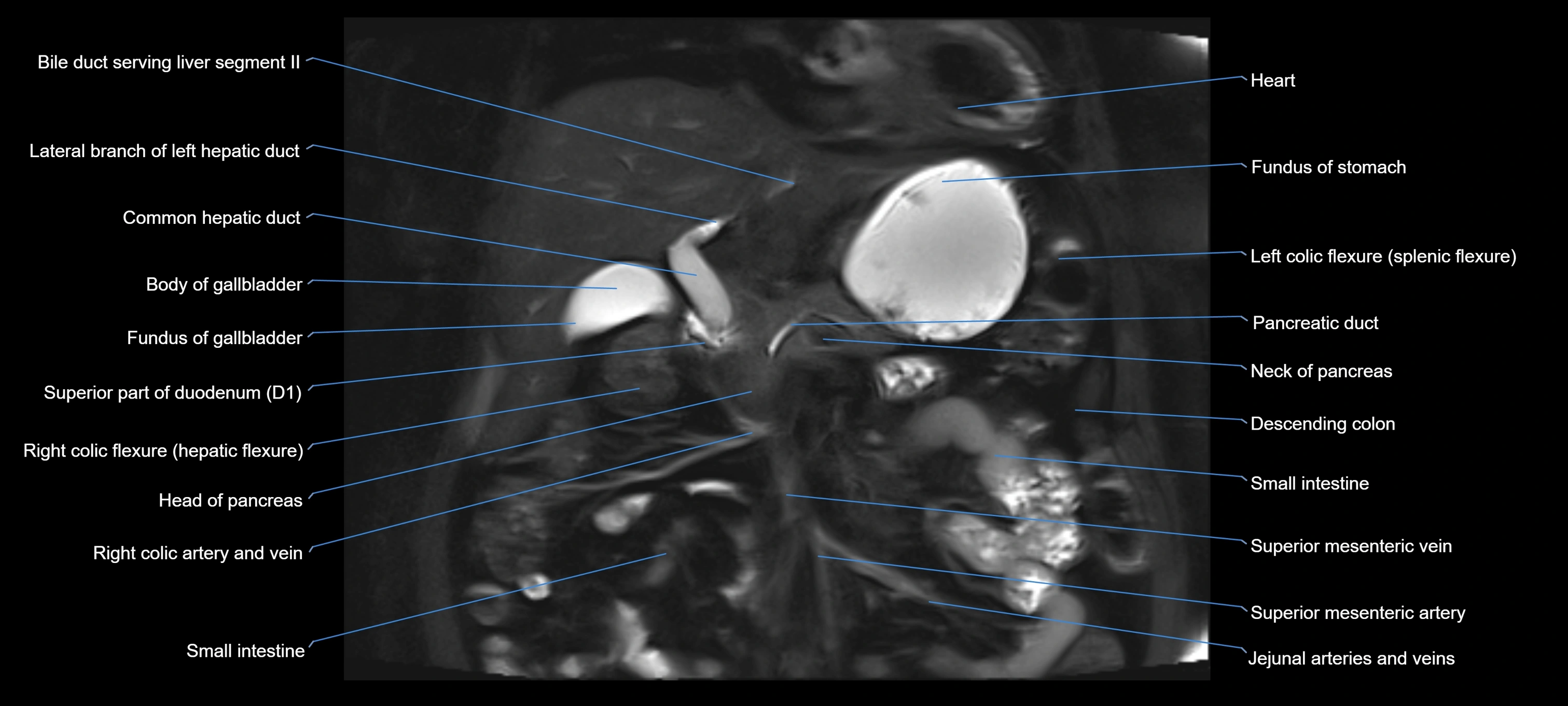
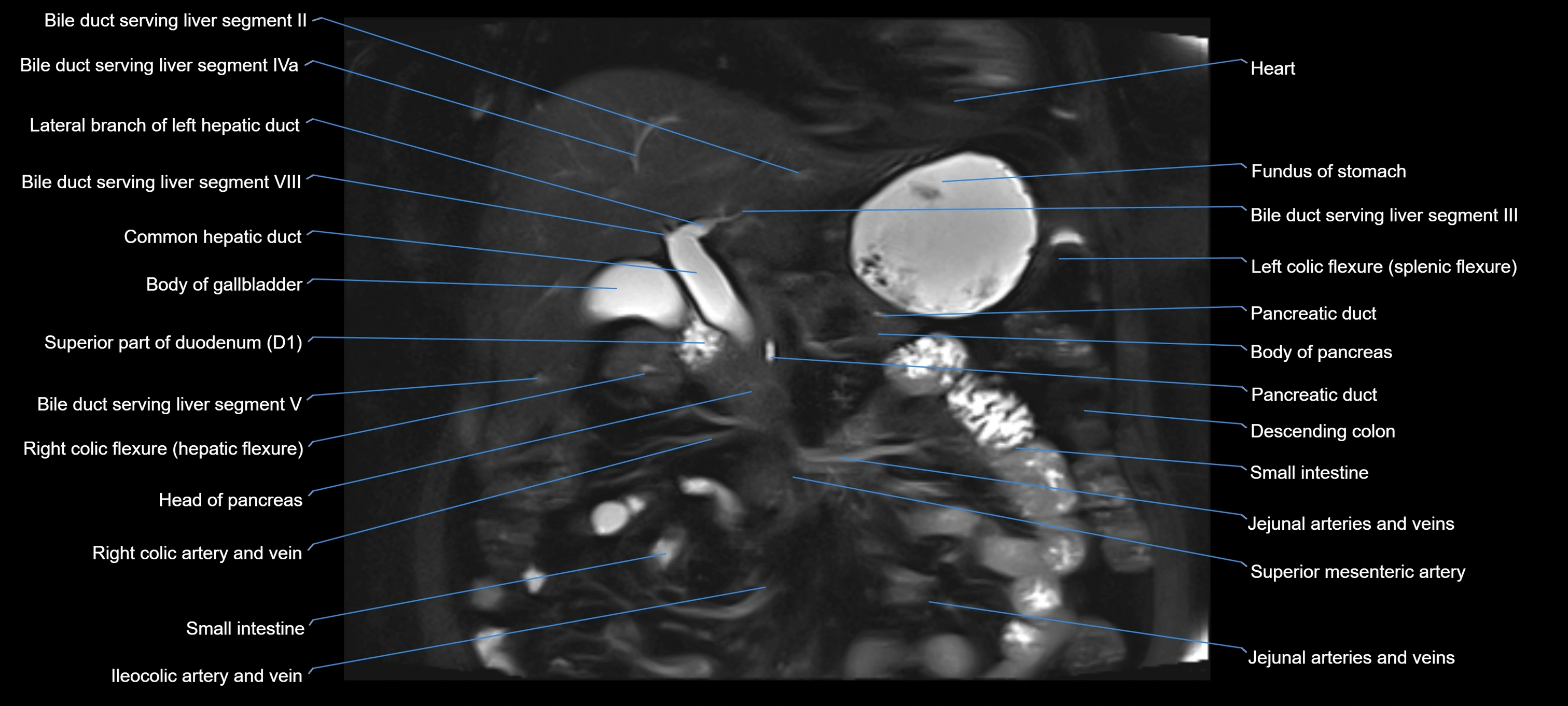
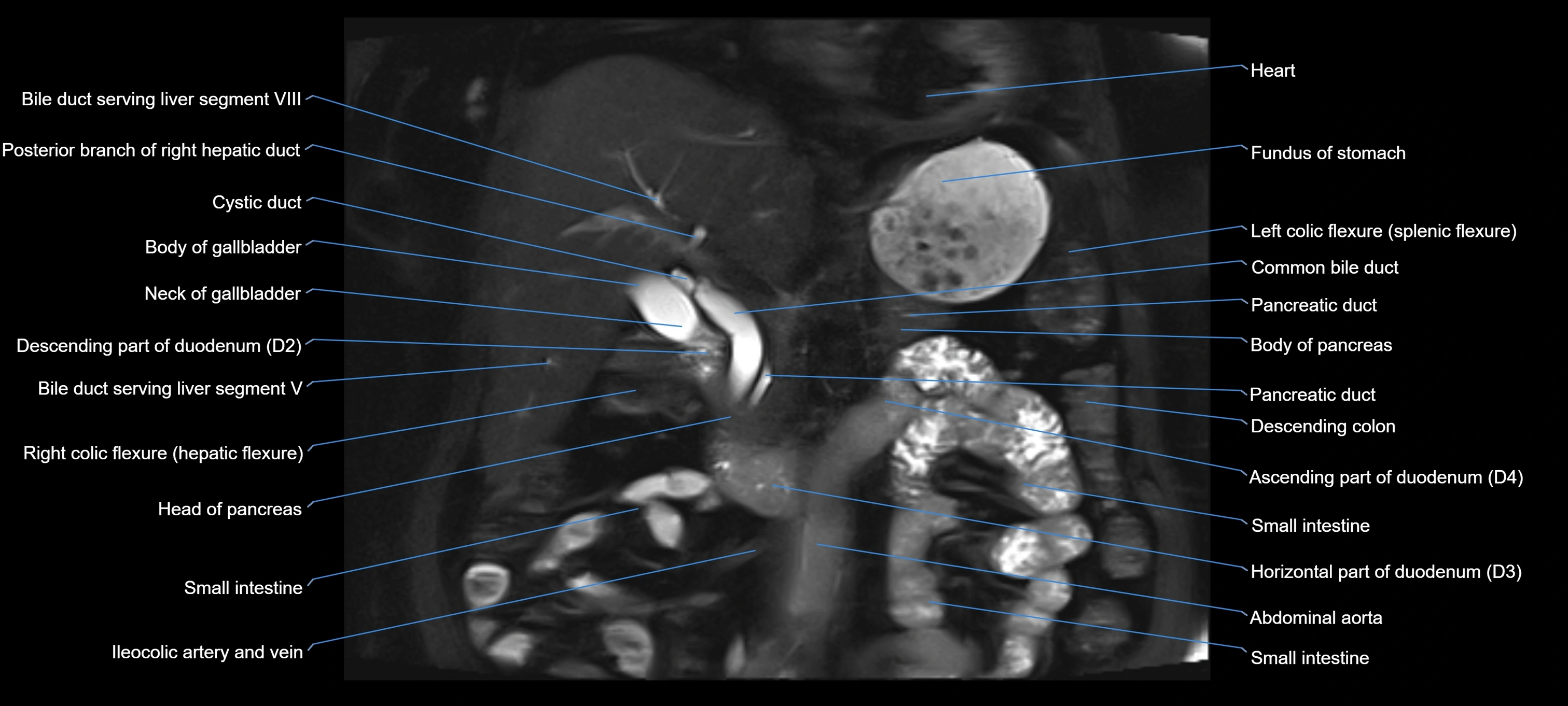
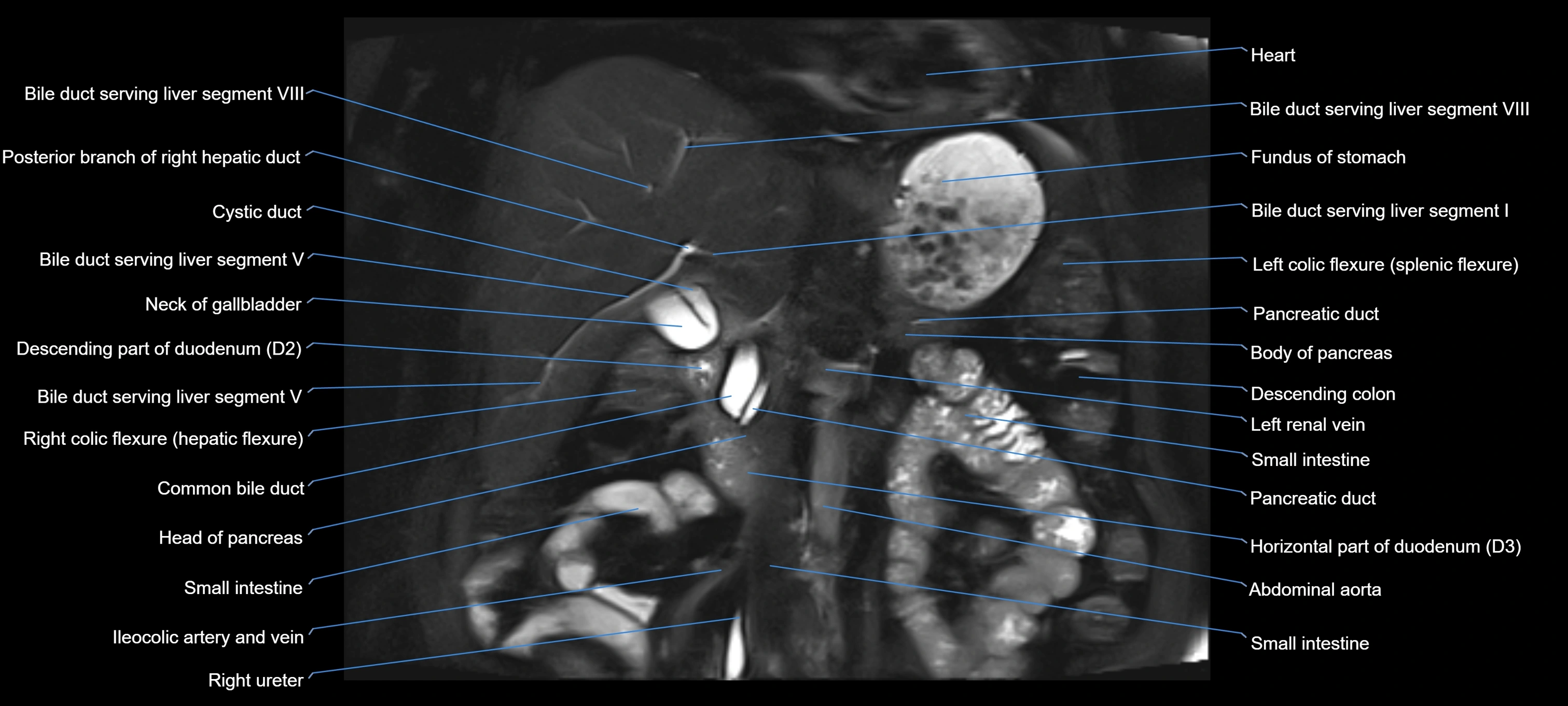
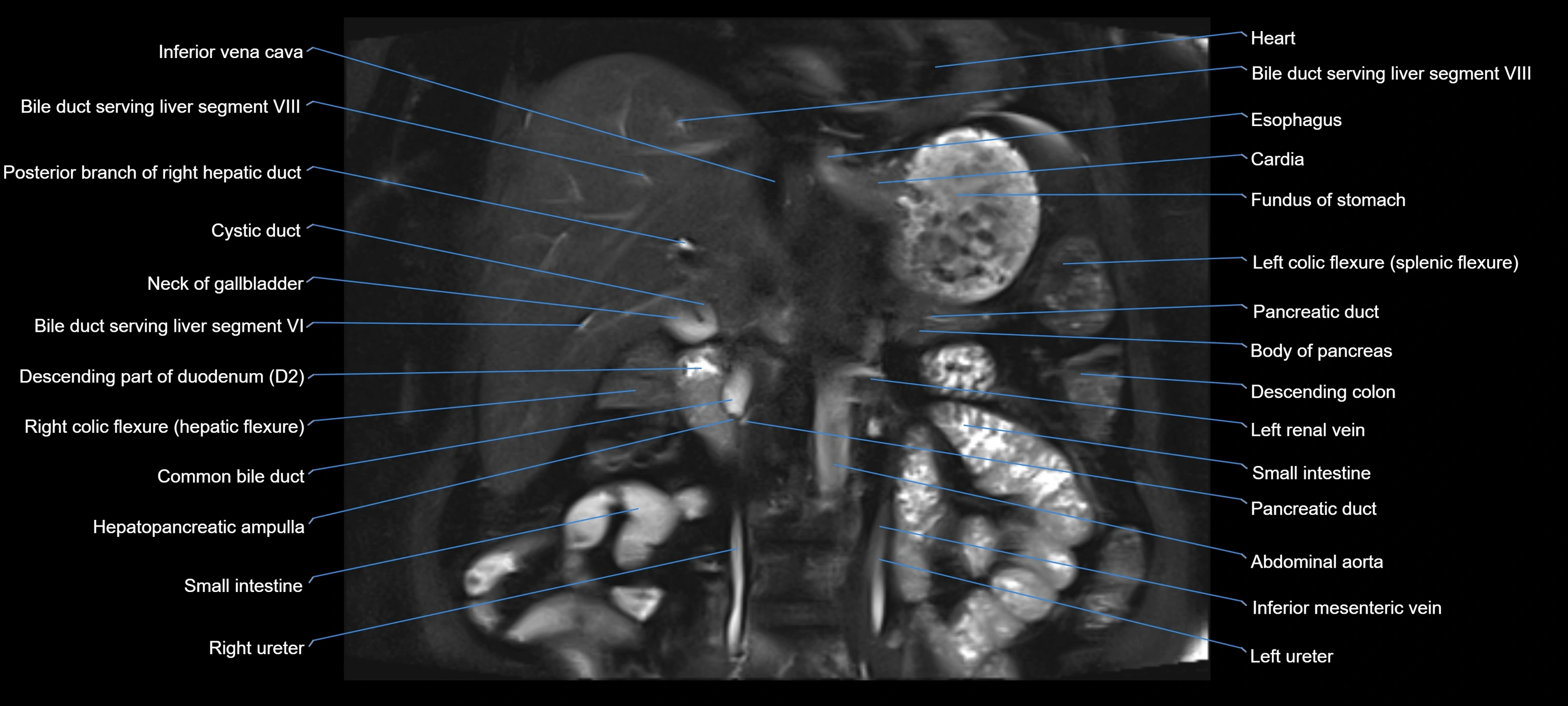
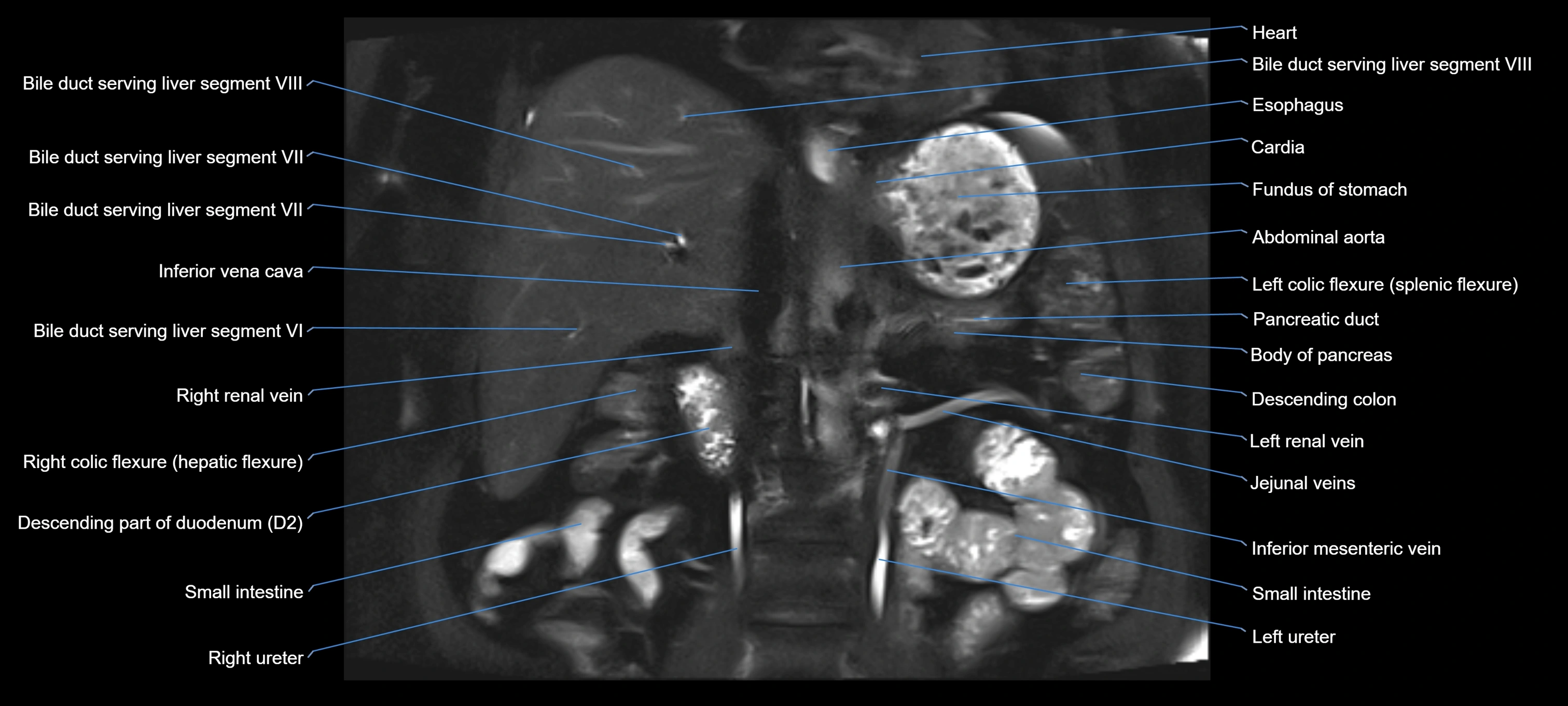
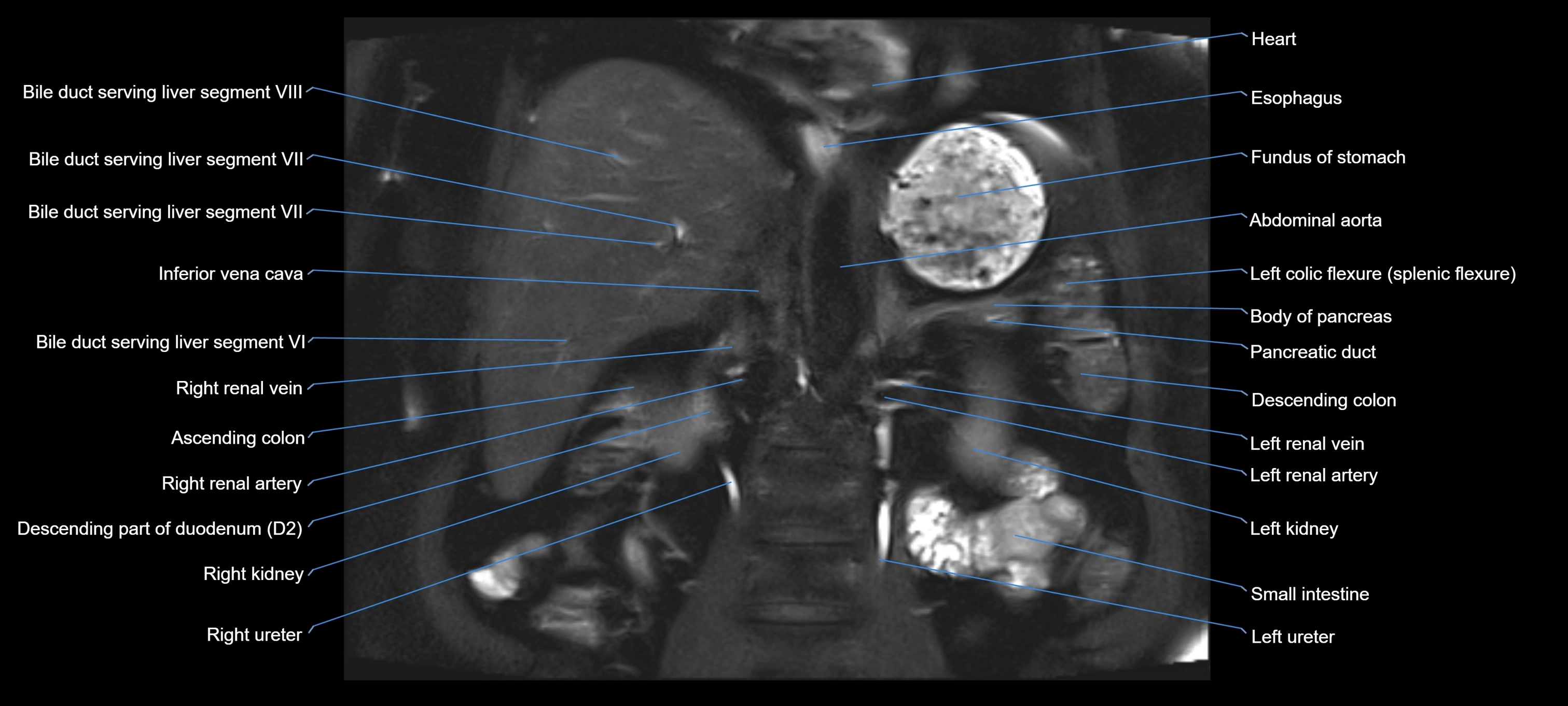
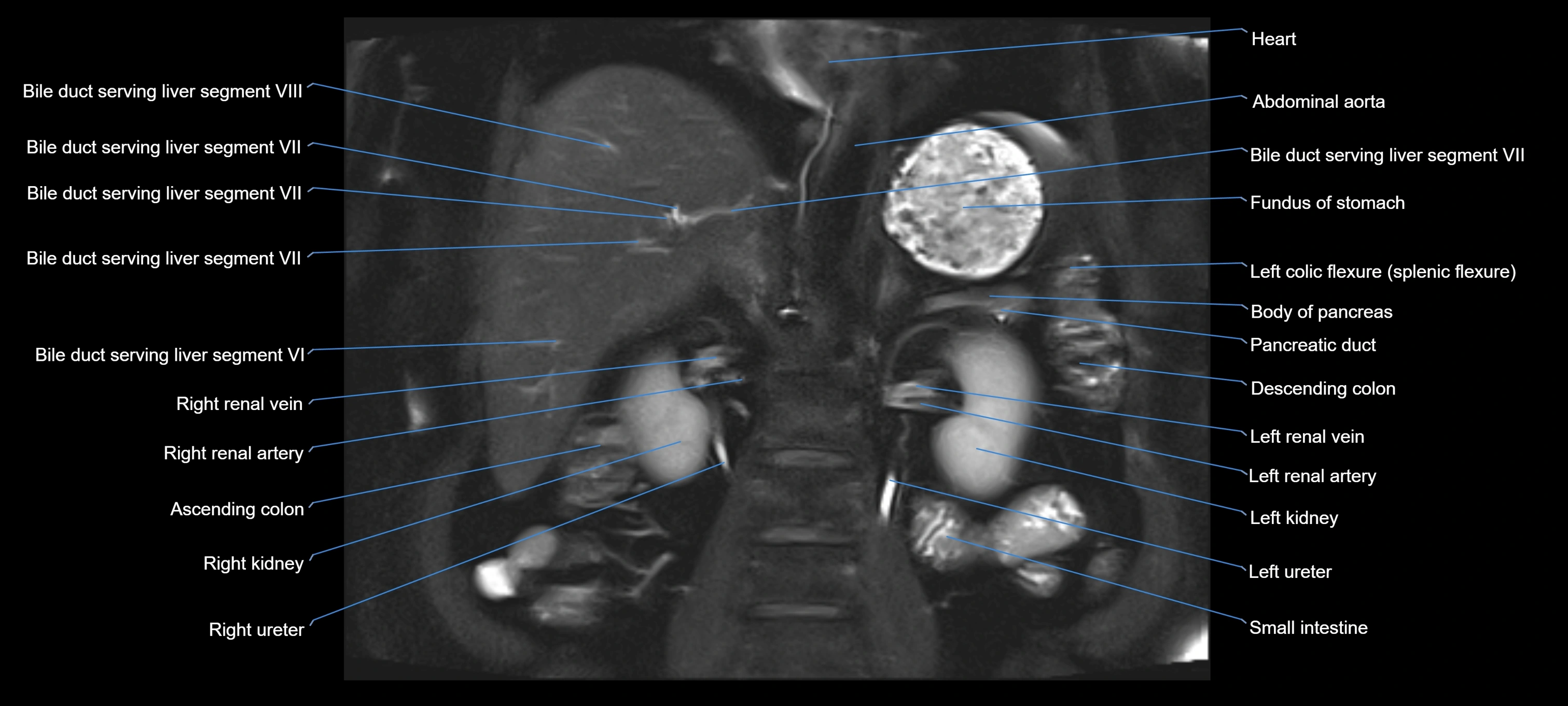
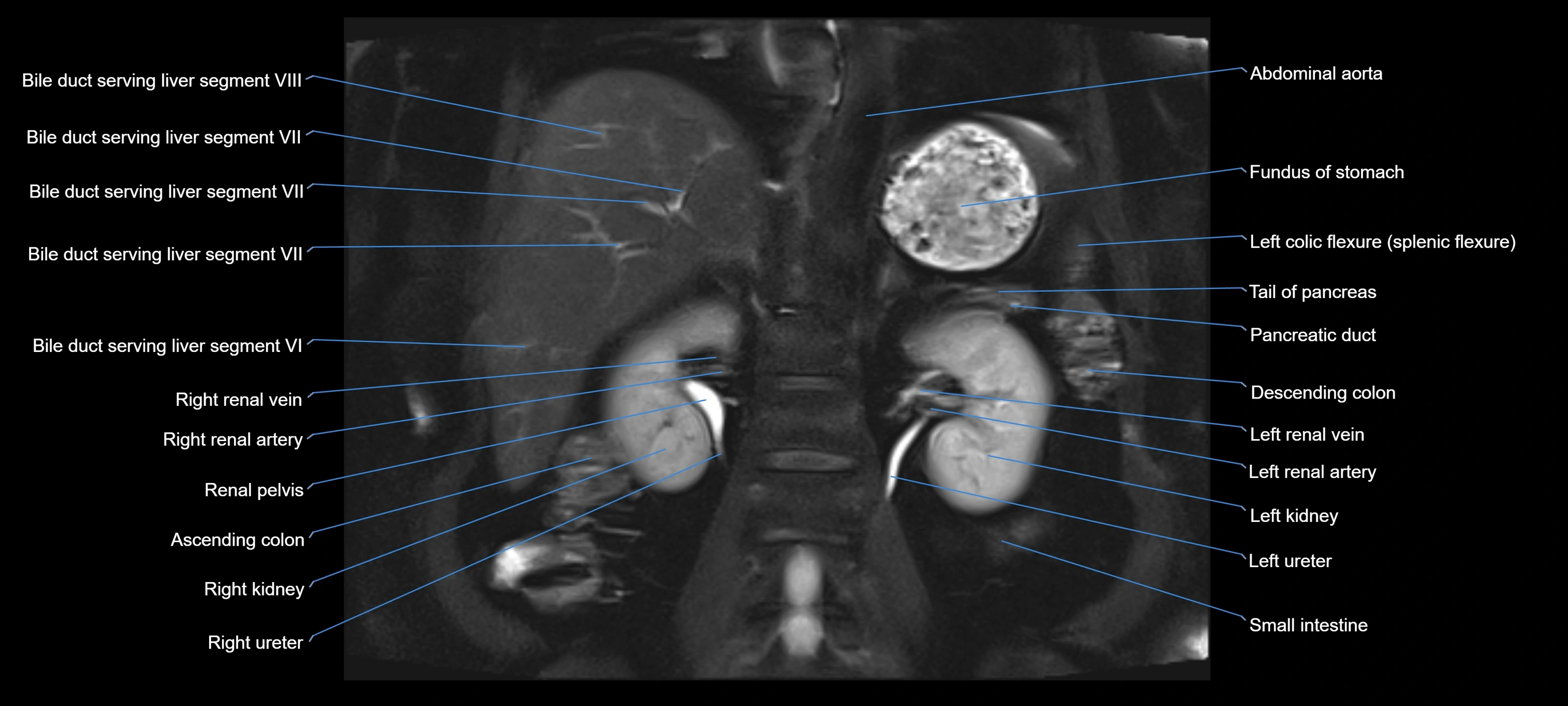
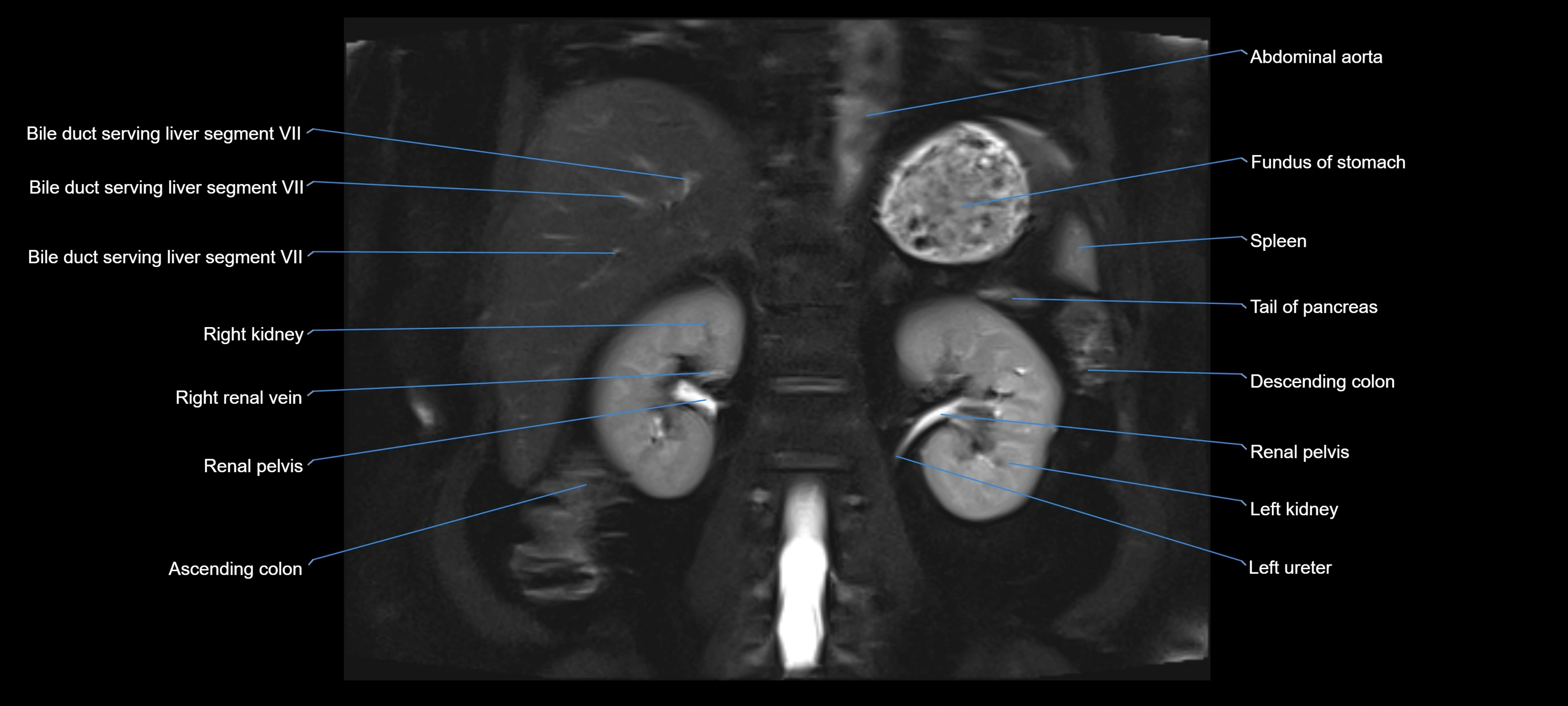
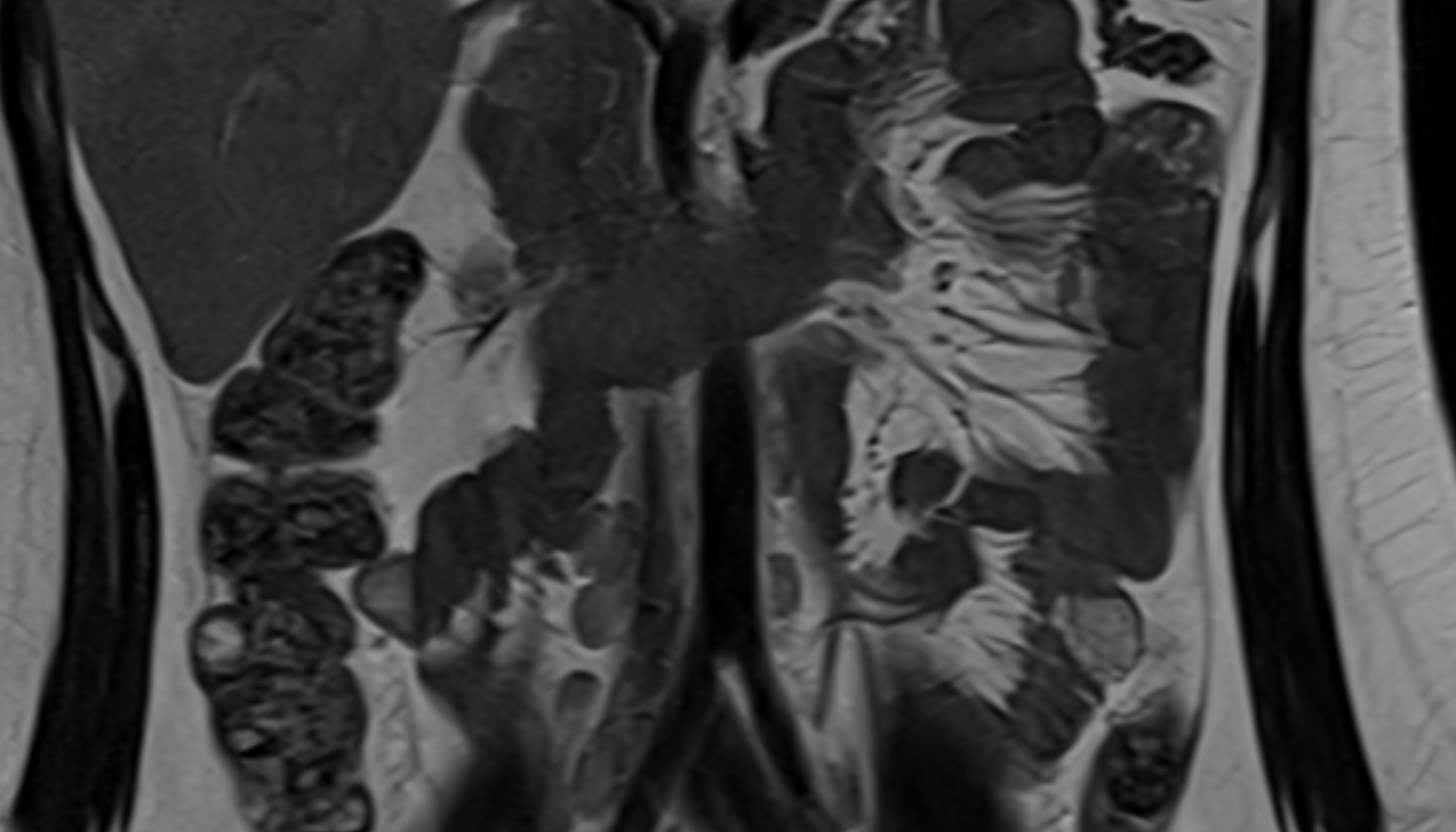
MRI image