Topic
The accessory cephalic vein is a variable superficial vein of the upper limb, typically draining the lateral and posterior aspects of the forearm and joining the cephalic vein near the cubital fossa or distal arm. It provides an important collateral drainage pathway for superficial venous return of the forearm.
It is often used as a landmark during venipuncture, vascular access creation (AV fistula), and venous graft harvesting. Due to its variable anatomy, precise imaging evaluation is essential before surgical or interventional procedures.
Synonyms
-
Lateral accessory vein of the forearm
-
Accessory cephalic branch
-
Superficial lateral forearm vein
Origin, Course, and Termination
-
Origin: Arises from the dorsal venous network of the hand, often from the lateral side of the dorsal venous arch.
-
Course:
-
Ascends along the lateral aspect of the forearm, anterior to the brachioradialis muscle.
-
In the distal or mid-forearm, it may communicate with the median cubital vein or directly with the cephalic vein.
-
Continues proximally on the radial border of the forearm and sometimes runs superficial to the lateral cutaneous nerve.
-
-
Termination:
-
Joins the cephalic vein just below or in the region of the cubital fossa; occasionally drains higher into the arm or shoulder region.
-
Relations
-
Anteriorly: Superficial fascia and skin of the lateral forearm
-
Posteriorly: Brachioradialis muscle and lateral antebrachial cutaneous nerve
-
Medially: Communicating veins from the dorsal venous network or cephalic vein
-
Laterally: Radial artery (deep), separated by fascia
Variations
-
May be absent, duplicated, or have multiple tributaries.
-
Sometimes continues as a dominant lateral forearm vein, replacing part of the cephalic vein.
-
May drain into the median cubital vein instead of the cephalic.
Function
-
Superficial venous drainage: Drains the lateral and posterior surfaces of the forearm and hand.
-
Collateral flow: Acts as an auxiliary route for venous return when the cephalic or median cubital vein is compromised.
-
Clinical relevance: Commonly used for venipuncture, catheterization, or venous grafts in reconstructive and vascular surgery.
Clinical Significance
-
Venipuncture site: Readily accessible and often used for IV lines or blood sampling.
-
AV fistula formation: Serves as an alternate venous channel for dialysis access creation.
-
Venous insufficiency or thrombosis: Slow flow or stasis may lead to thrombophlebitis or varicosities.
-
Surgical relevance: Important to identify during cephalic vein dissection to prevent iatrogenic injury.
-
Imaging role: MRI/MRA and CTA essential for assessing venous patency, flow, thrombosis, and anatomic variants.
MRI Appearance
-
T1-weighted images:
-
Flowing blood: low signal (flow void) due to rapid venous flow.
-
Slow-flowing blood: may appear intermediate-to-bright signal, sometimes mimicking soft tissue structures.
-
Vein wall: thin, low signal; perivenous fat is bright.
-
Thrombus: variable signal—acute (isointense), subacute (bright).
-
-
T2-weighted images:
-
Fast flow: dark flow void.
-
Slow-flowing blood: intermediate-to-bright signal, especially on long TE sequences.
-
Thrombus or wall thickening: hyperintense or intermediate signal.
-
Perivenous edema: bright signal in surrounding soft tissues.
-
-
STIR:
-
Normal vein: dark to intermediate signal (depending on flow velocity).
-
Slow-flowing blood: may appear intermediate or mildly hyperintense.
-
Thrombosed segments or inflammation: bright hyperintense wall or perivenous signal.
-
-
Proton Density Fat-Saturated (PD FS):
-
Normal vein lumen: intermediate-to-dark signal.
-
Slow flow: may show moderate bright intraluminal signal due to sluggish venous return.
-
Thrombosis or inflammation: bright wall and surrounding soft tissue enhancement.
-
-
T1 Fat-Sat Post-Contrast:
-
Normal patent vein: uniform enhancement after gadolinium injection.
-
Thrombus: non-enhancing intraluminal filling defect.
-
Periphlebitis or thrombophlebitis: enhancing wall with surrounding soft-tissue stranding.
-
CT Appearance
Non-Contrast CT:
-
Vein lumen appears as a tubular soft-tissue density superficial to the brachioradialis.
-
Difficult to distinguish from adjacent soft tissue unless phleboliths or calcifications present.
-
Chronic thrombosis may show wall thickening or perivenous fat stranding.
Post-Contrast CT (standard):
-
Vein enhances homogeneously during venous or delayed phase imaging.
-
Thrombosis: intraluminal non-enhancing area with vein enlargement.
-
Helpful in evaluating venous patency before vascular access surgery.
CTA (CT Angiography / Venography) Appearance
-
Normal: Enhancing superficial vein along the lateral forearm joining the cephalic vein; well seen in venous phase CTA.
-
Thrombosis: non-enhancing segment or partial filling defect.
-
Varicosity: irregular, dilated, tortuous enhancing vein.
-
Surgical planning: CTA delineates vein course, diameter, and continuity with cephalic vein for fistula or graft creation.
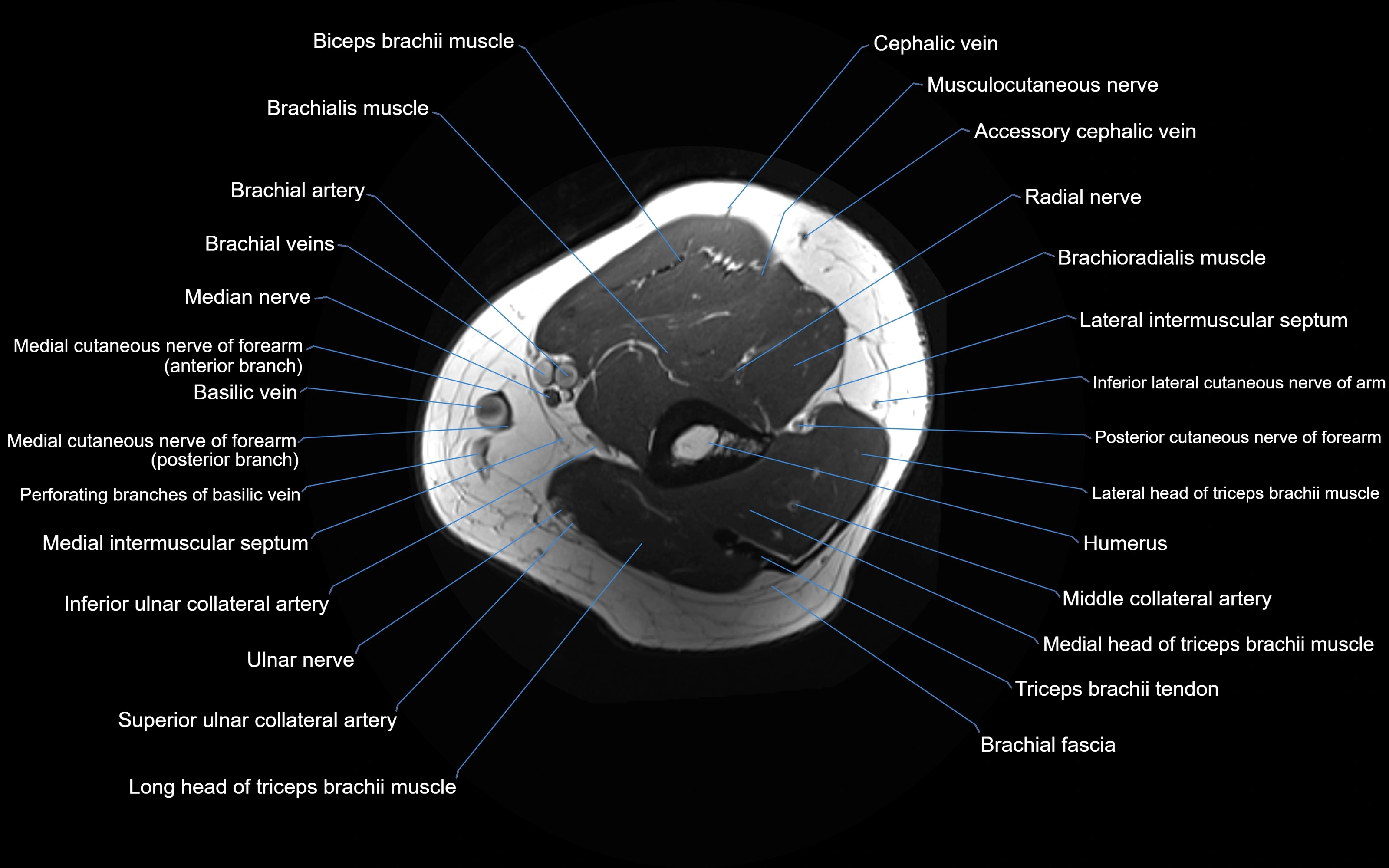
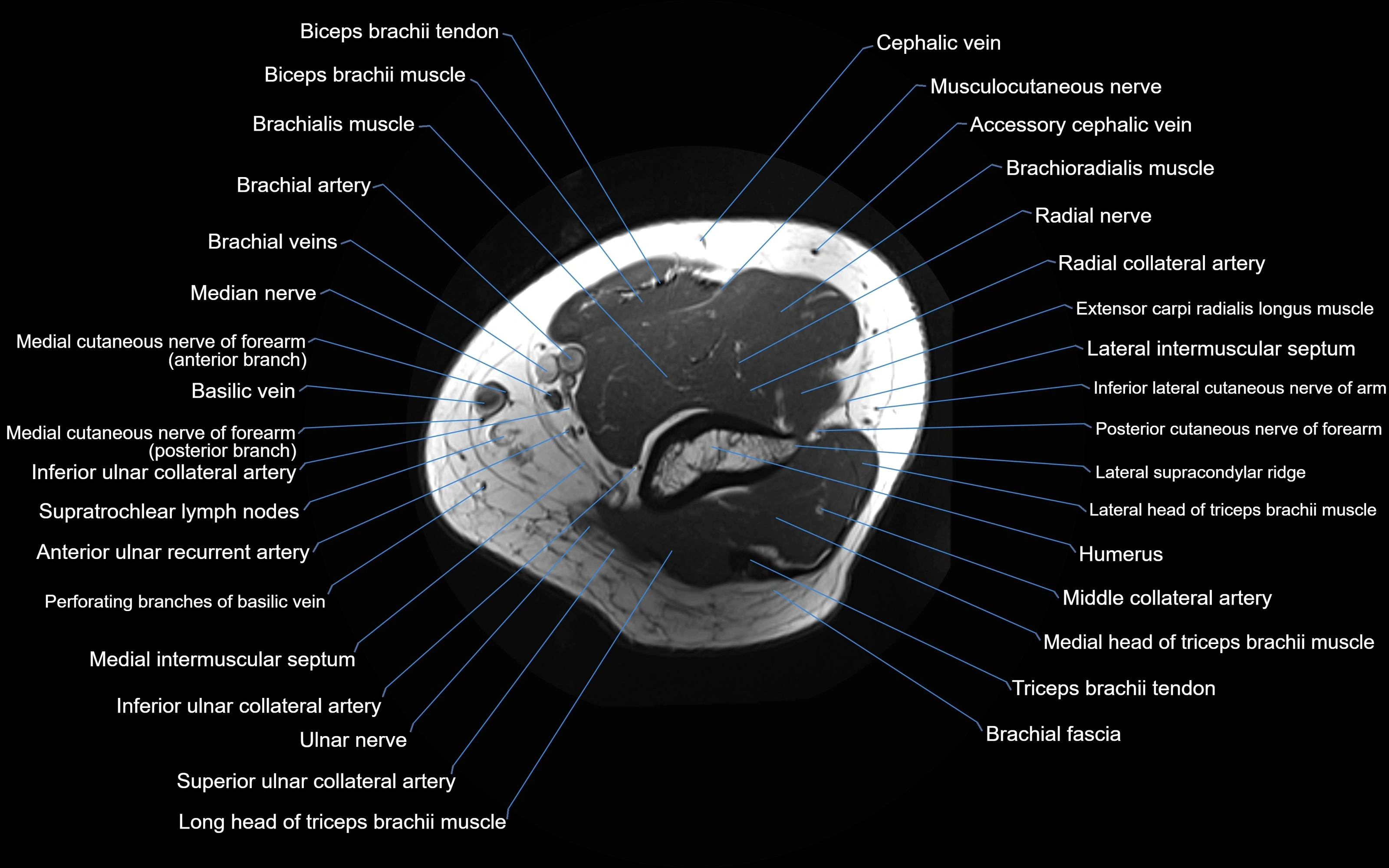
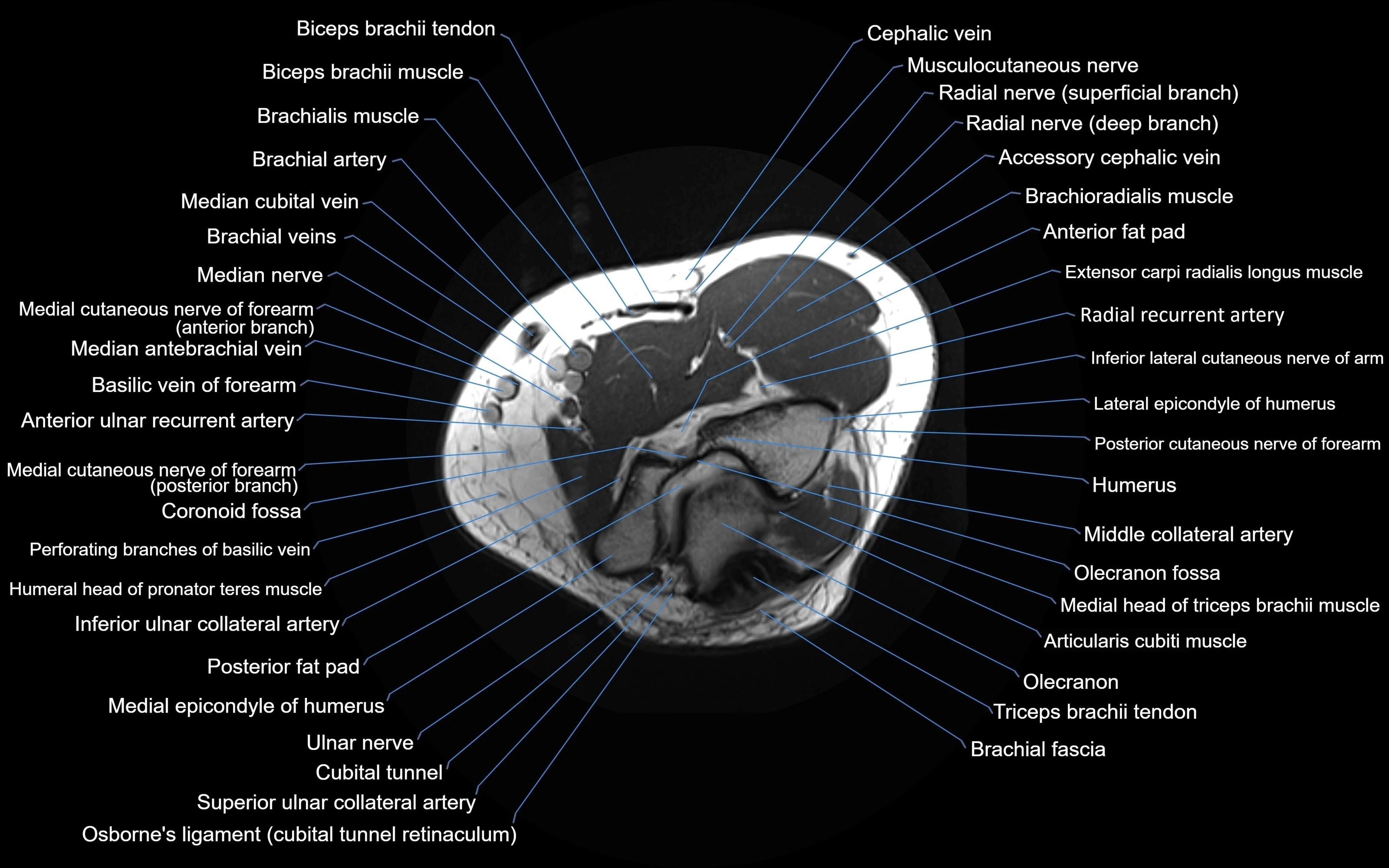
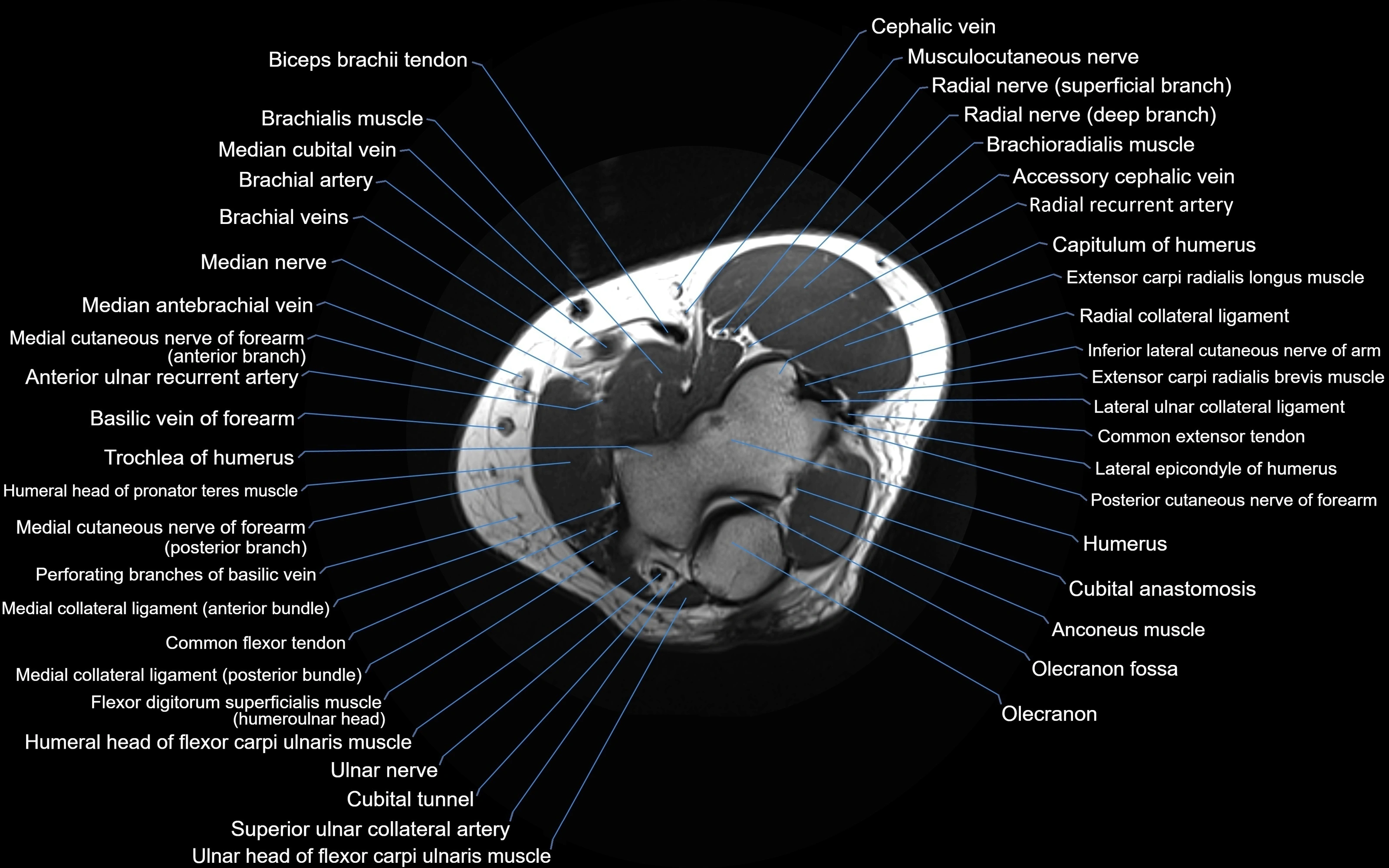
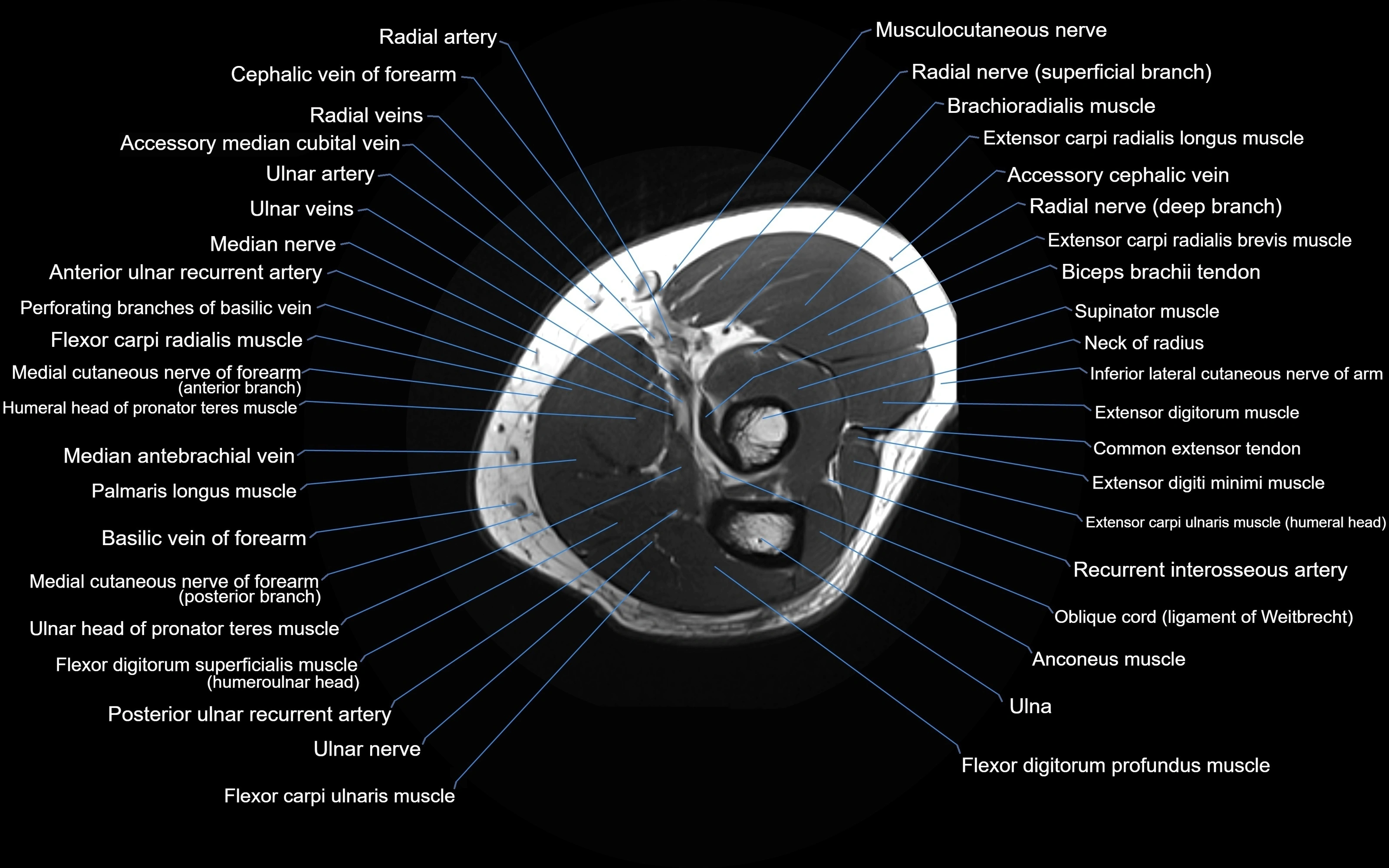
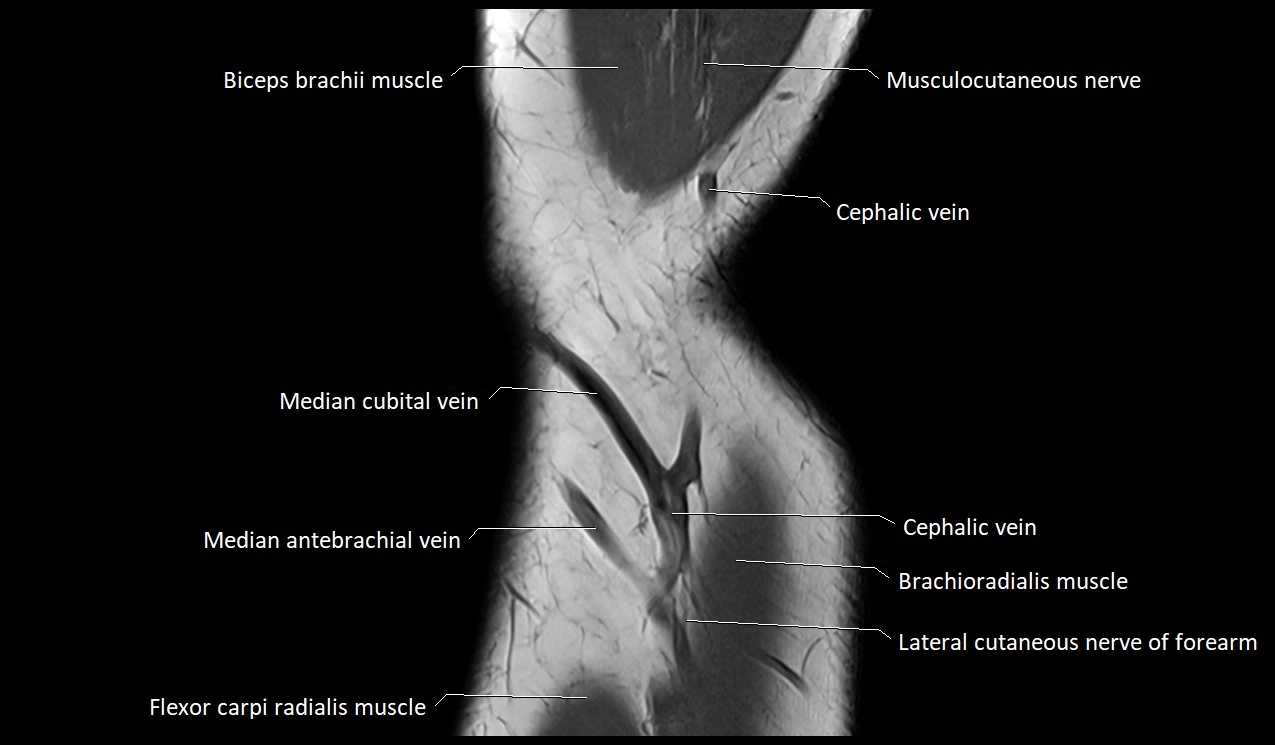
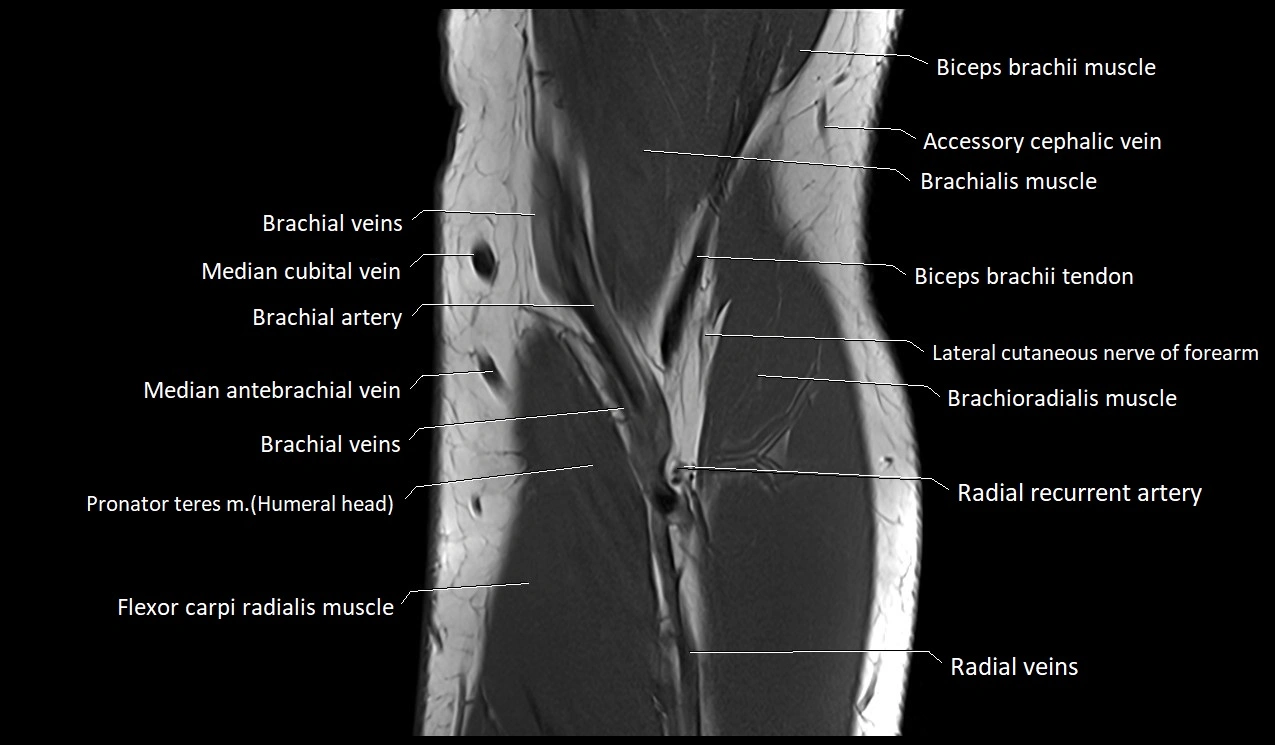
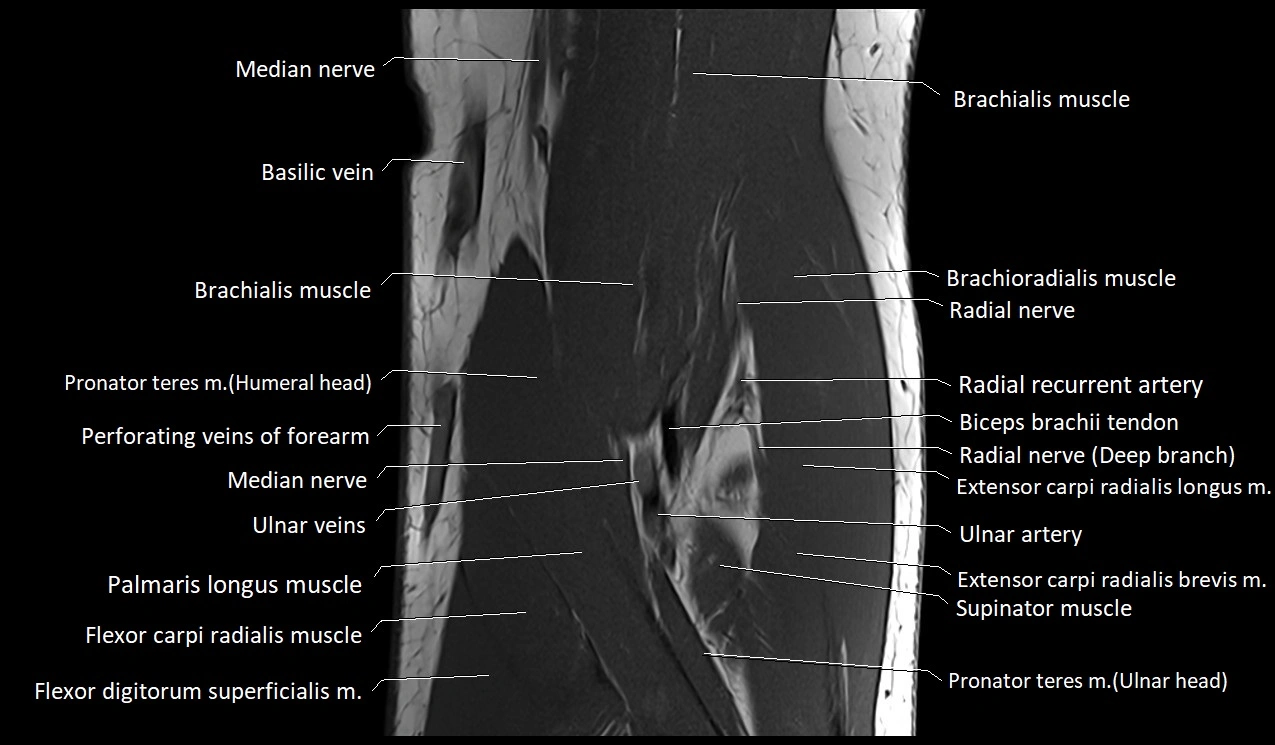
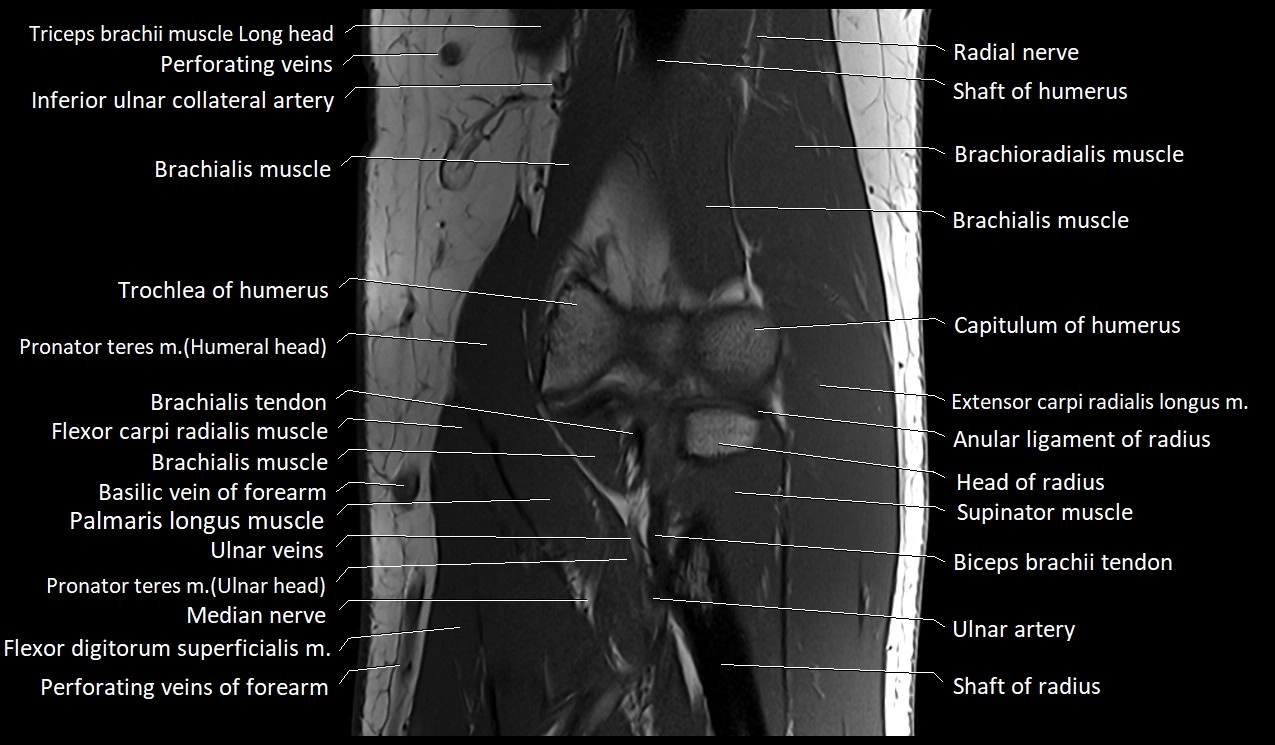
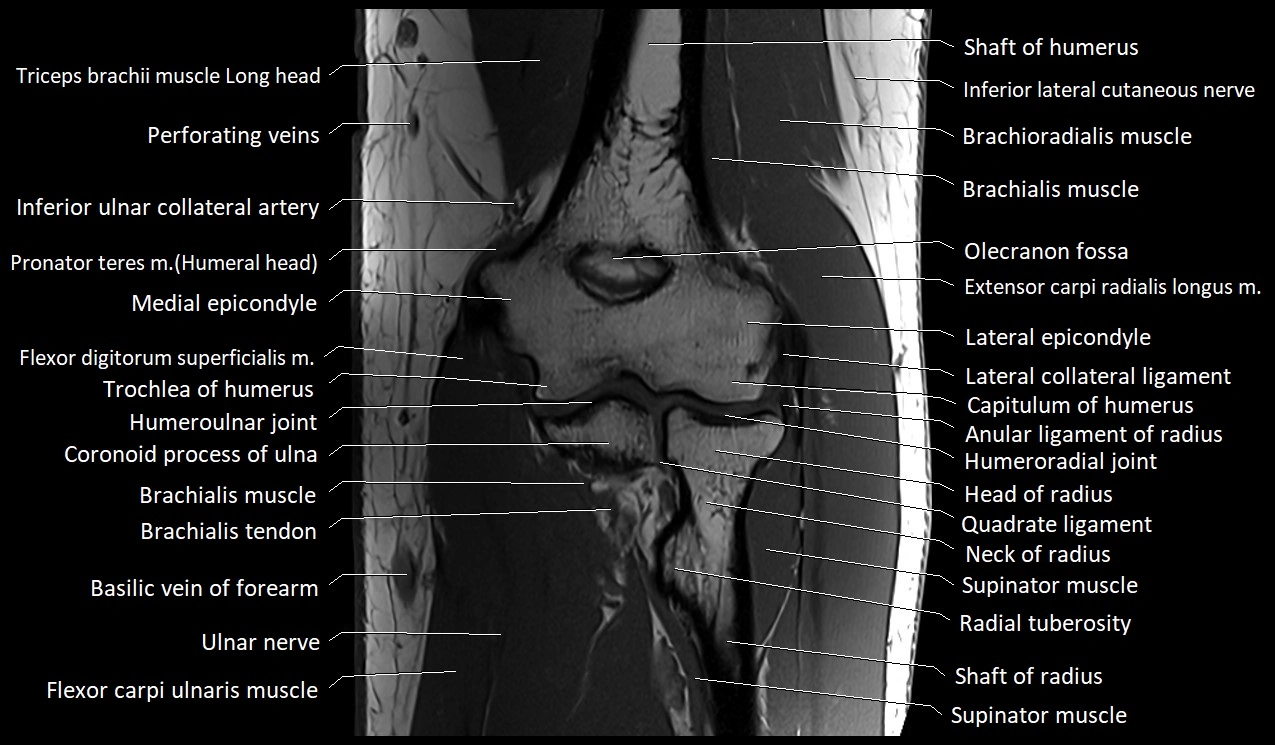
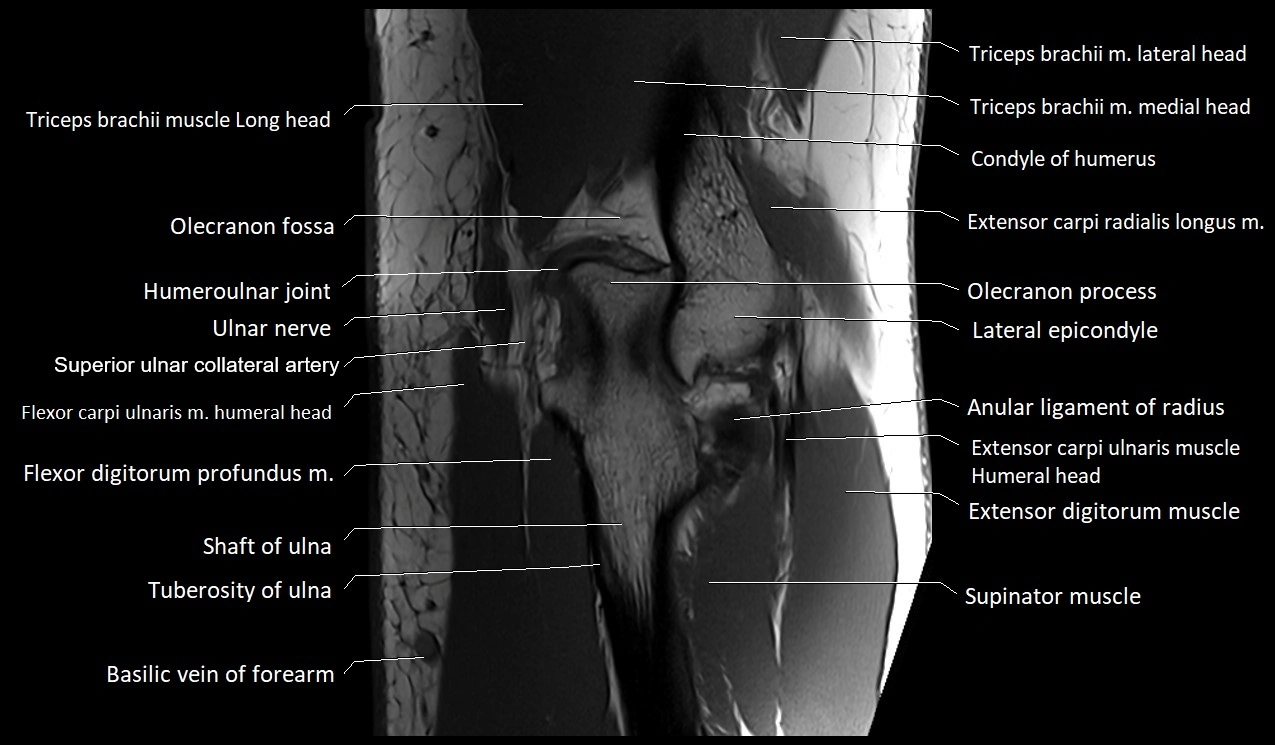
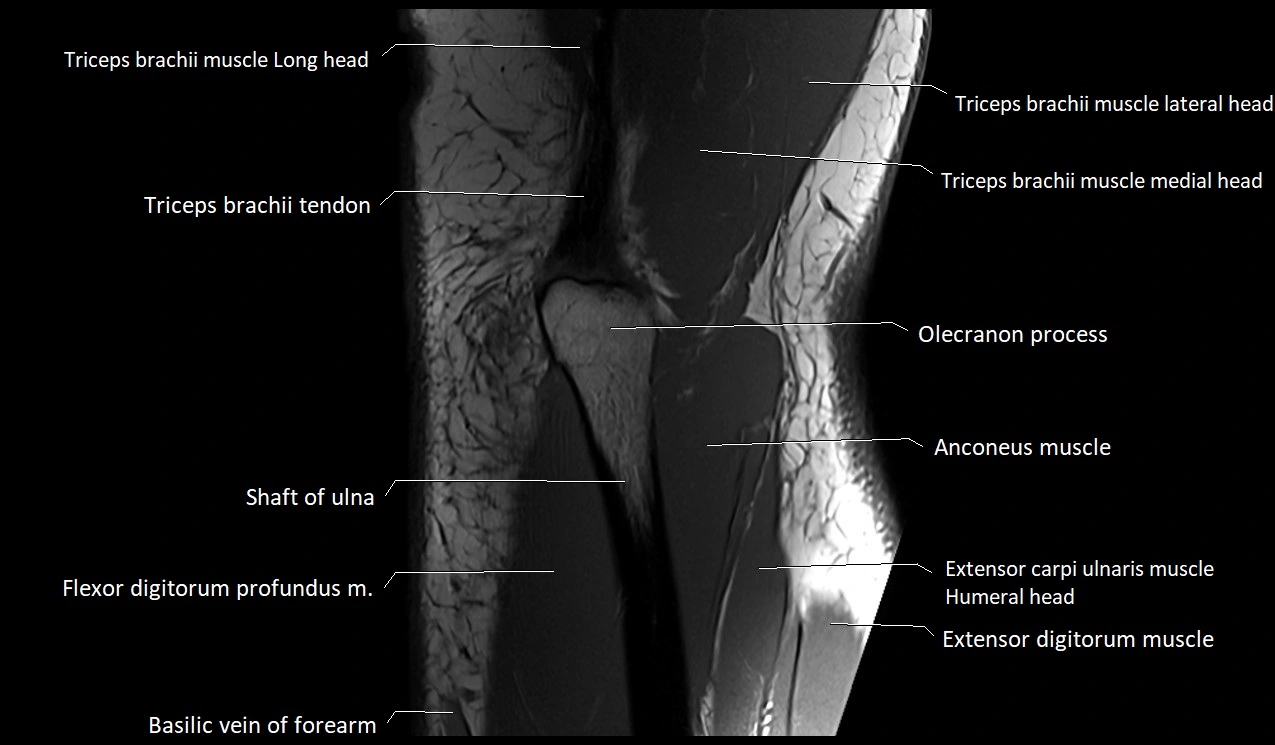
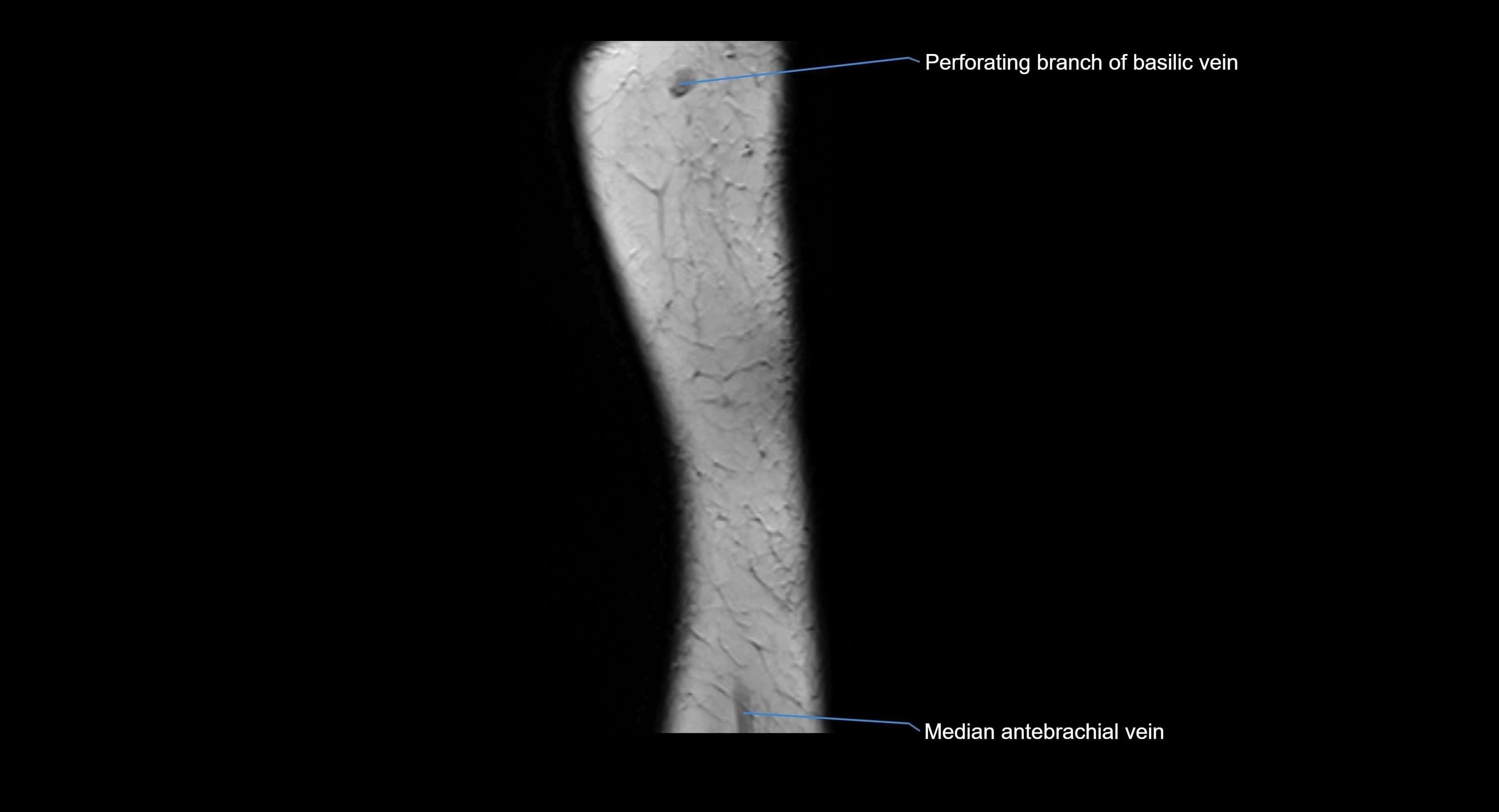
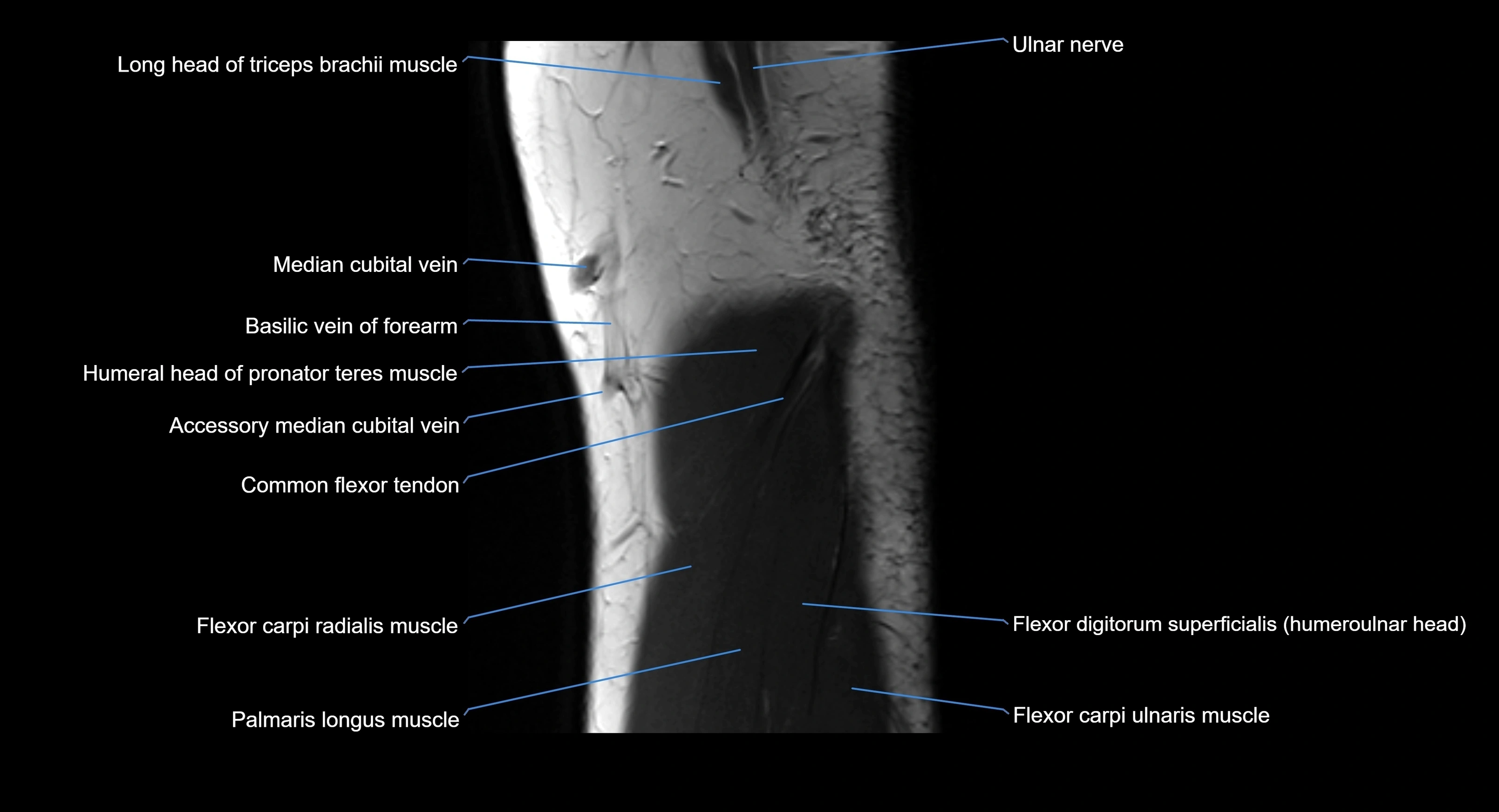
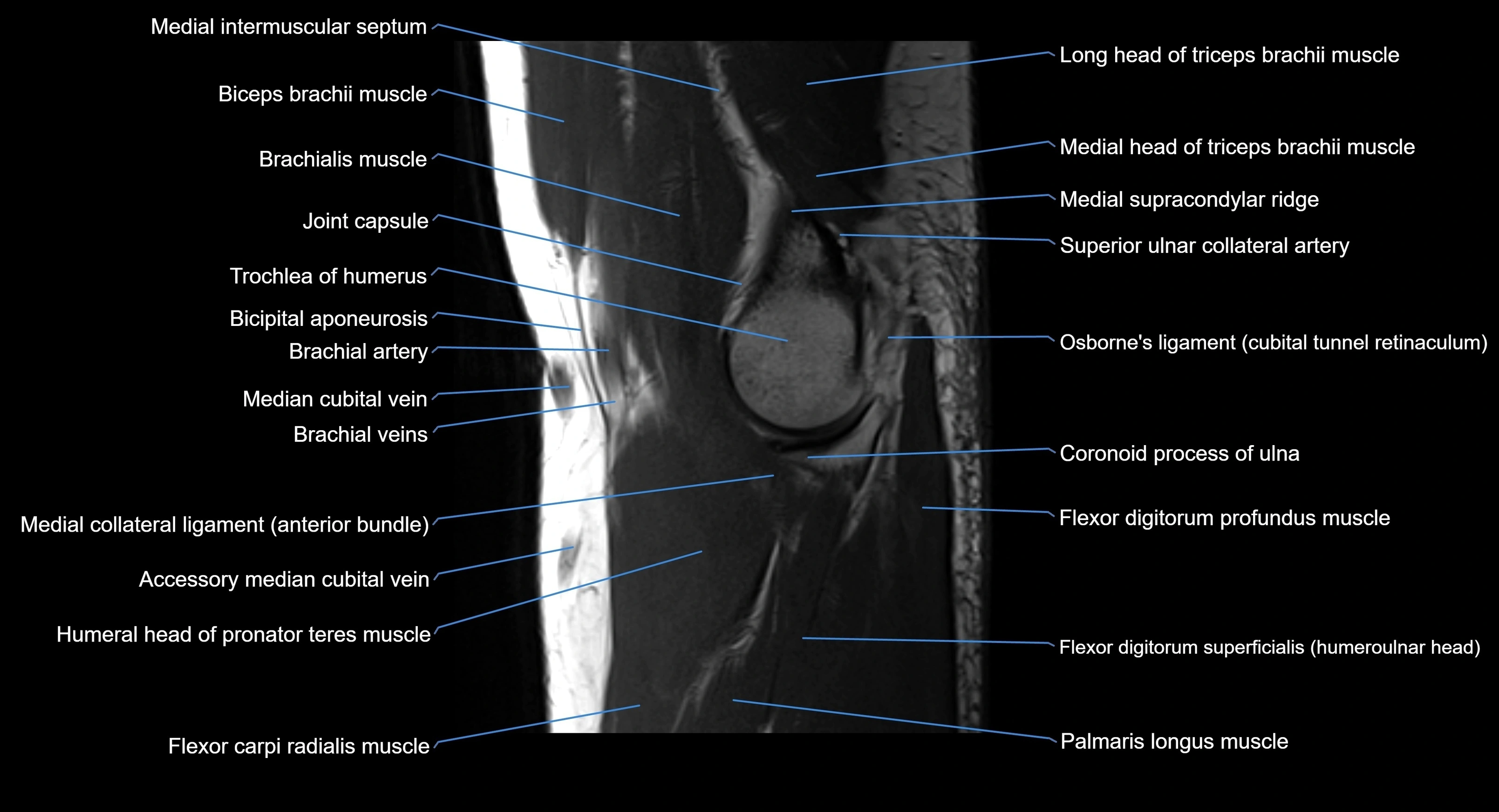
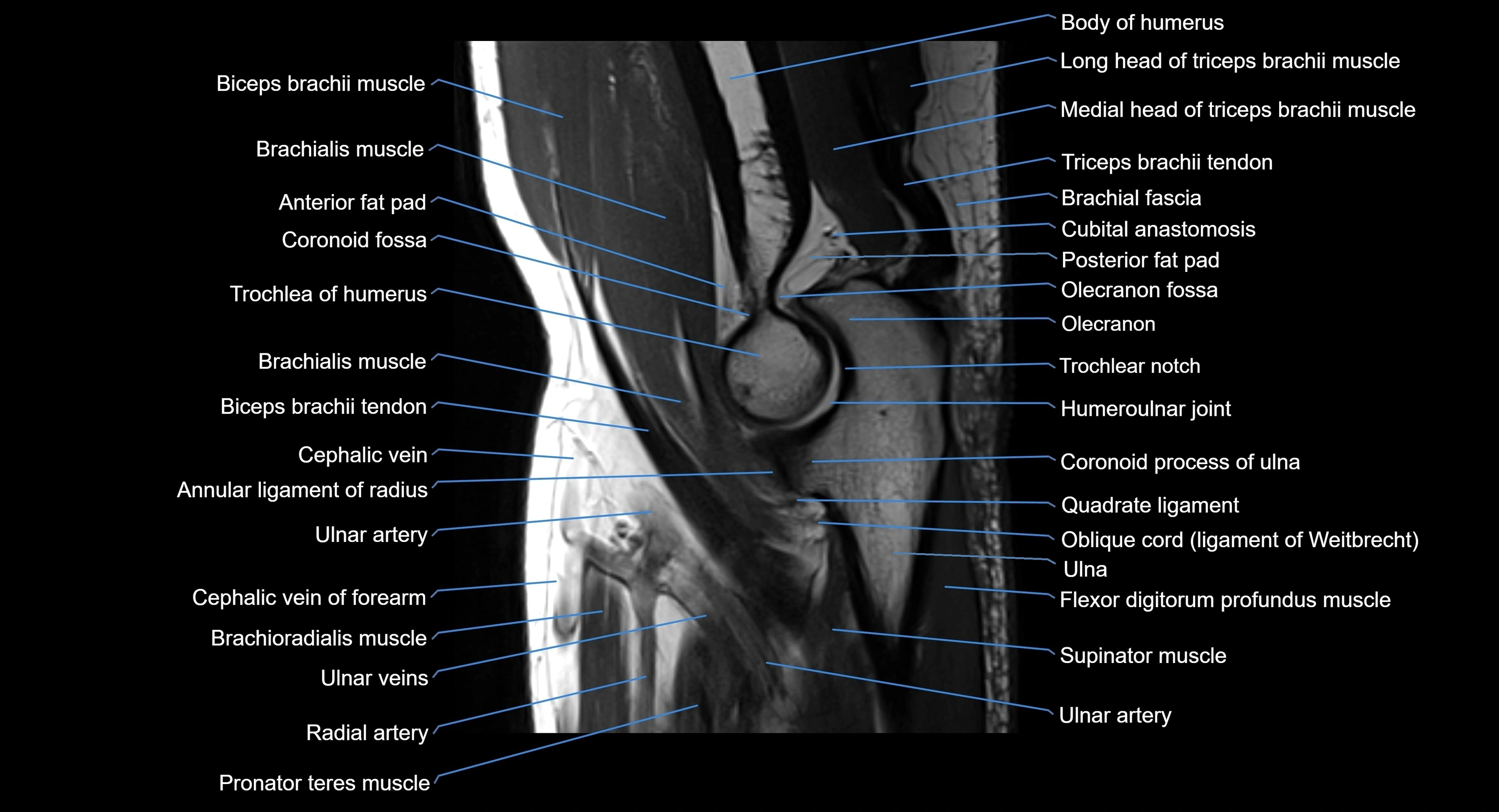
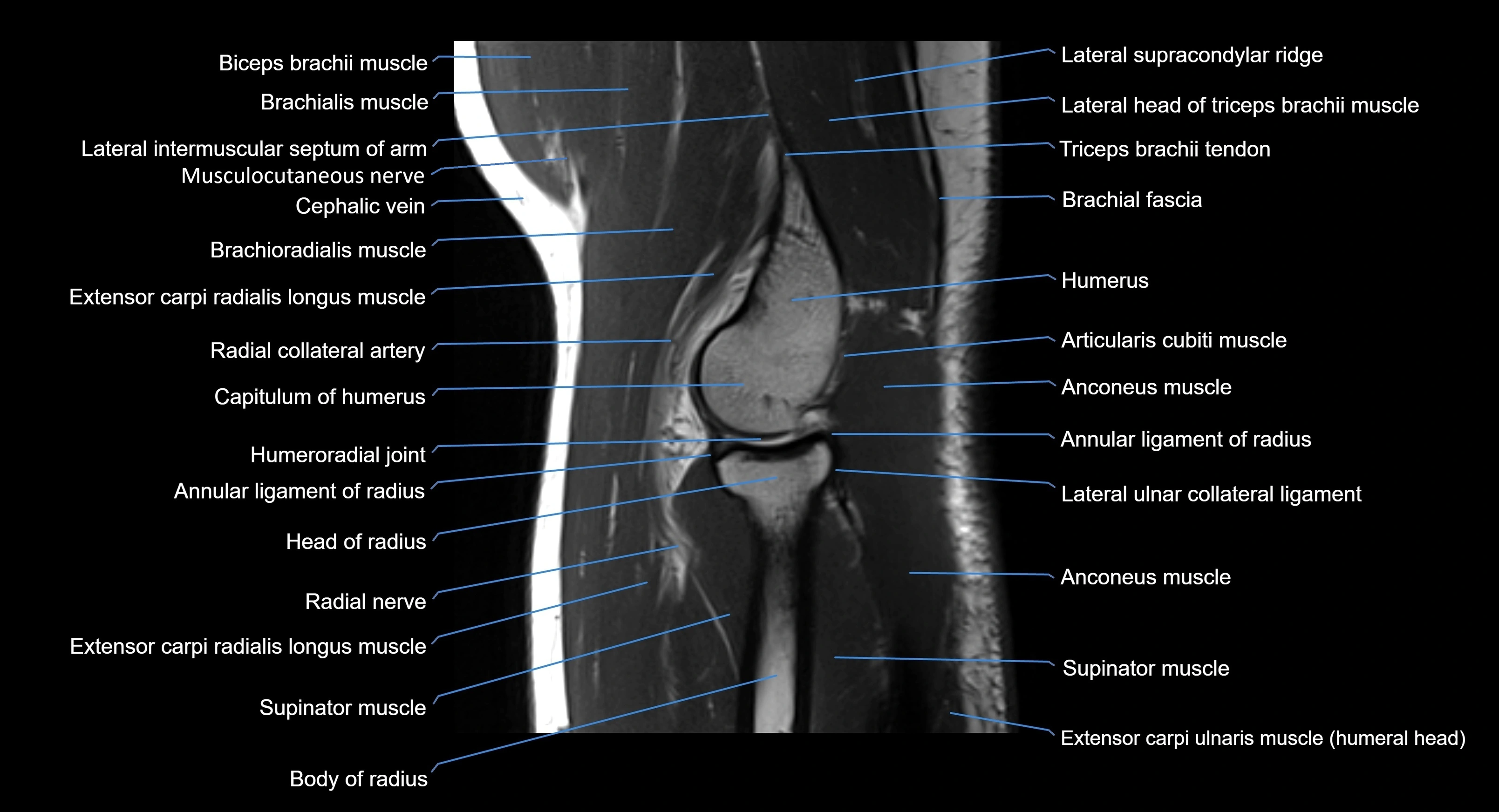
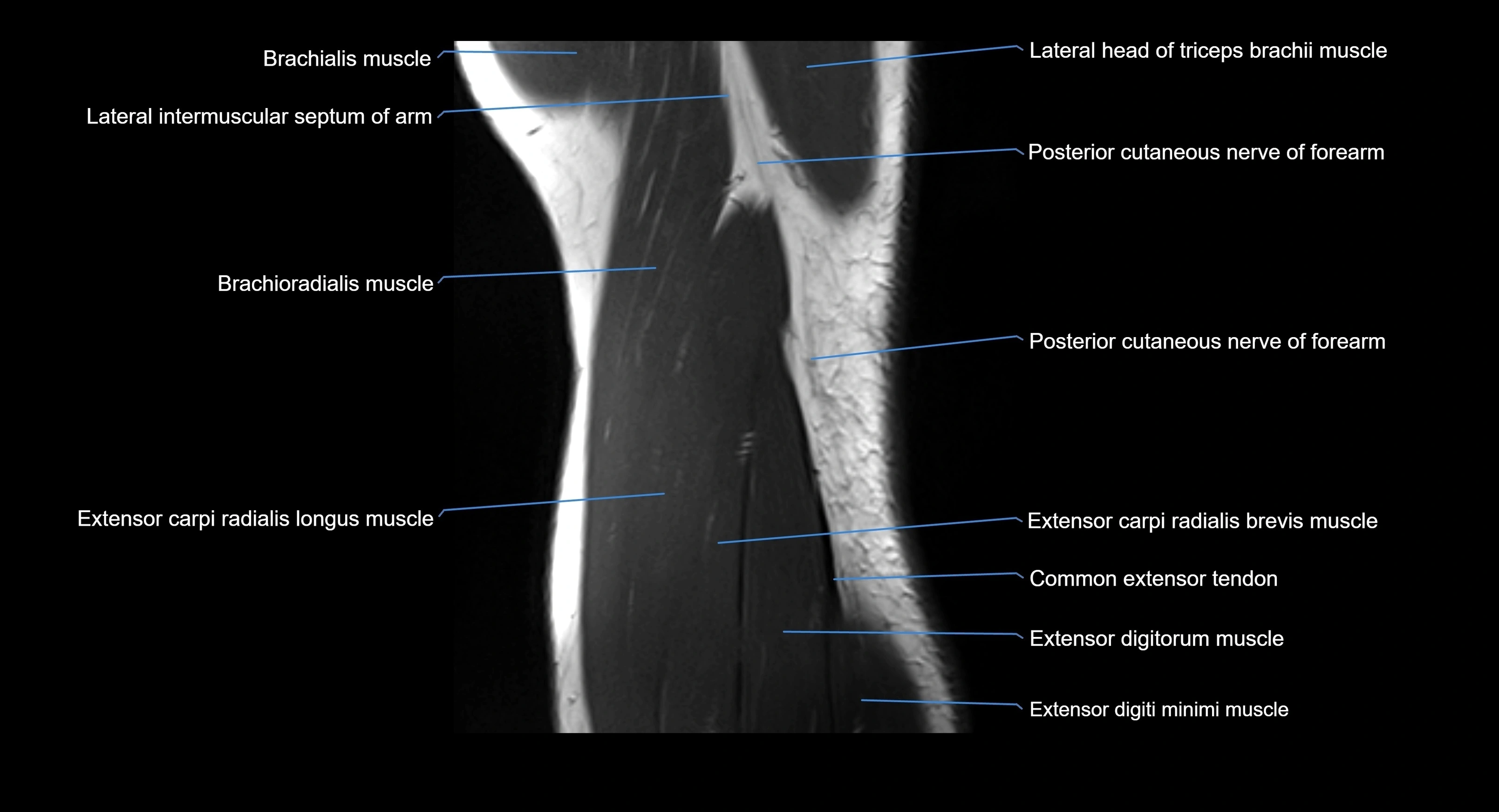
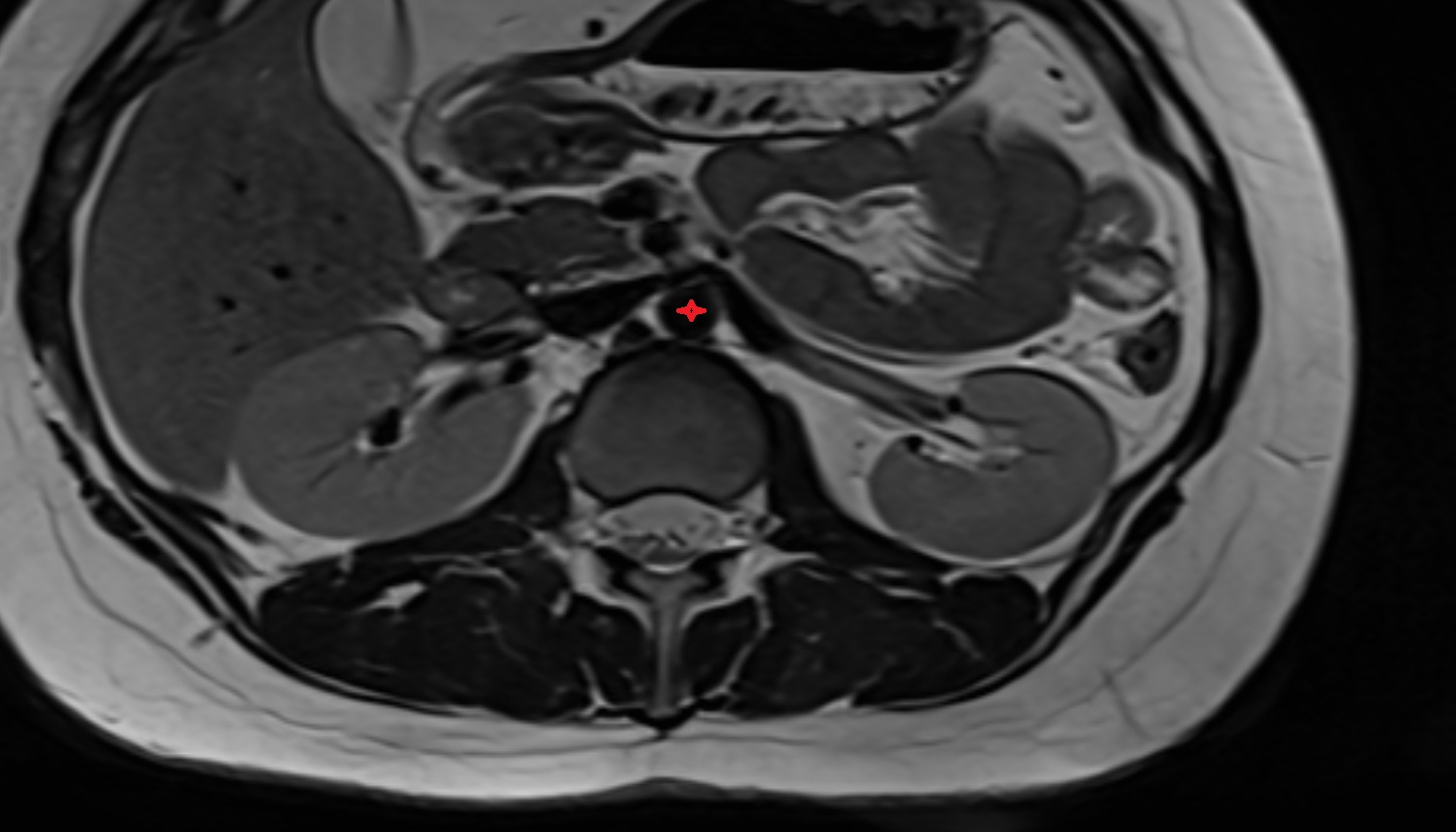
MRI image

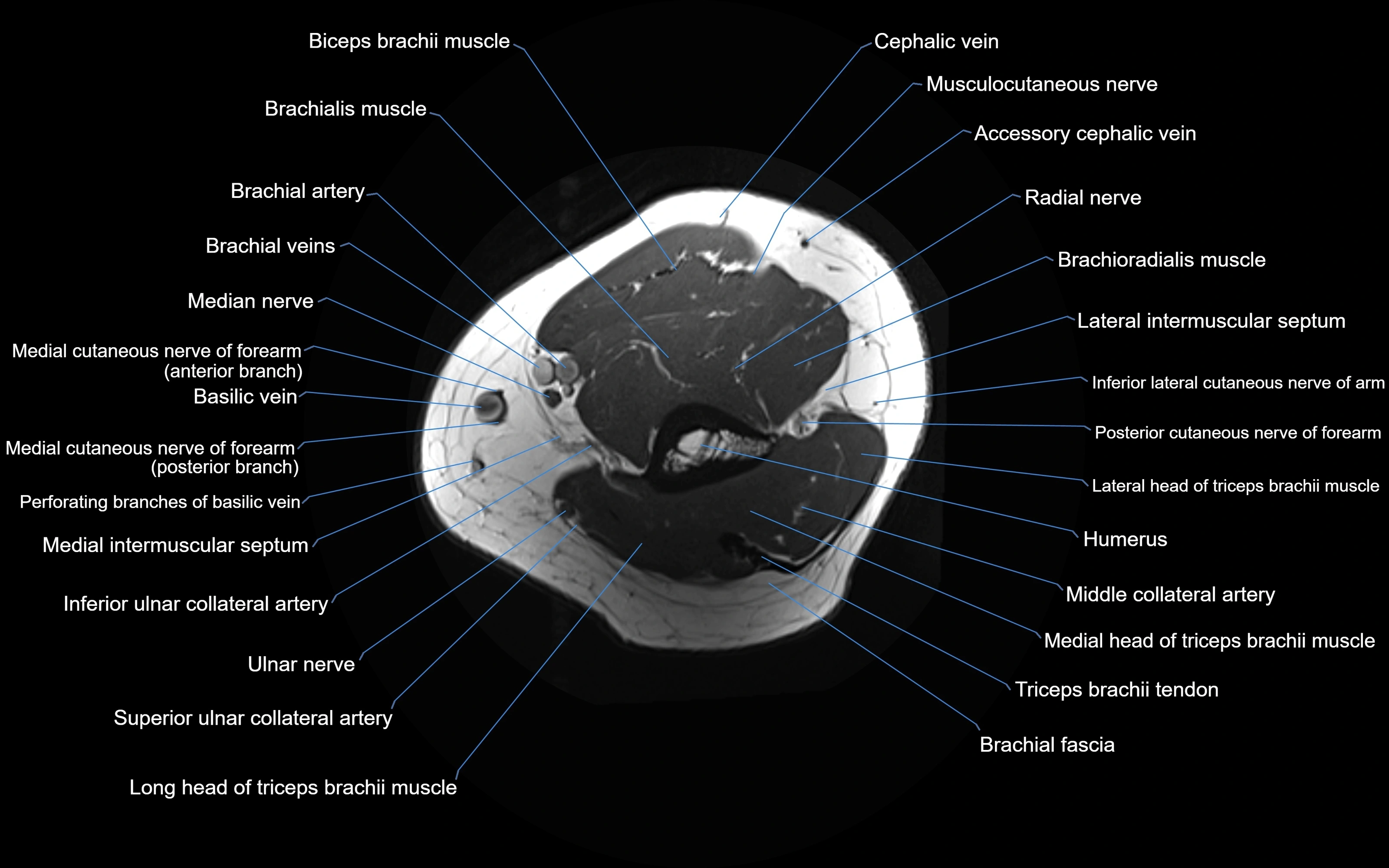
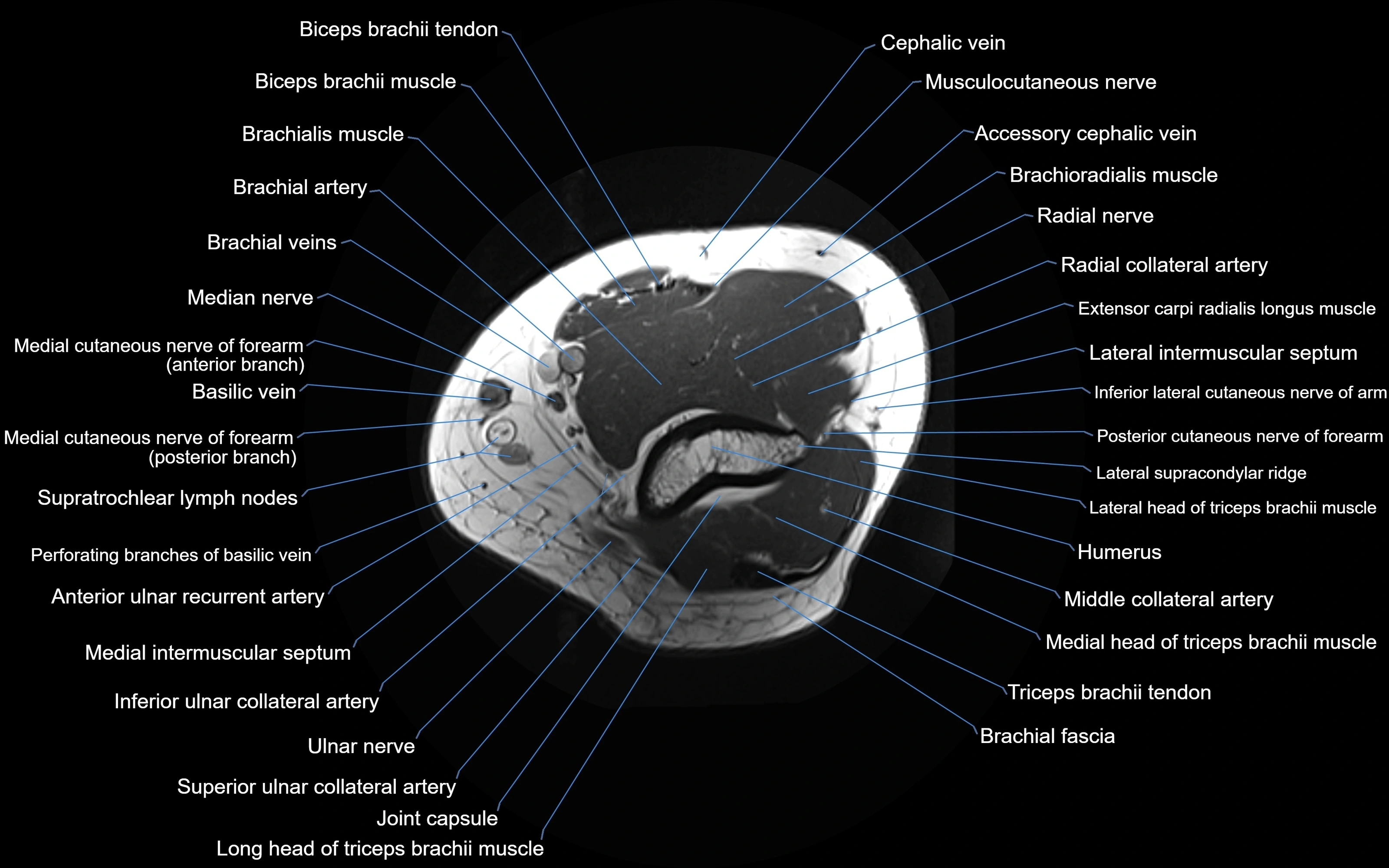
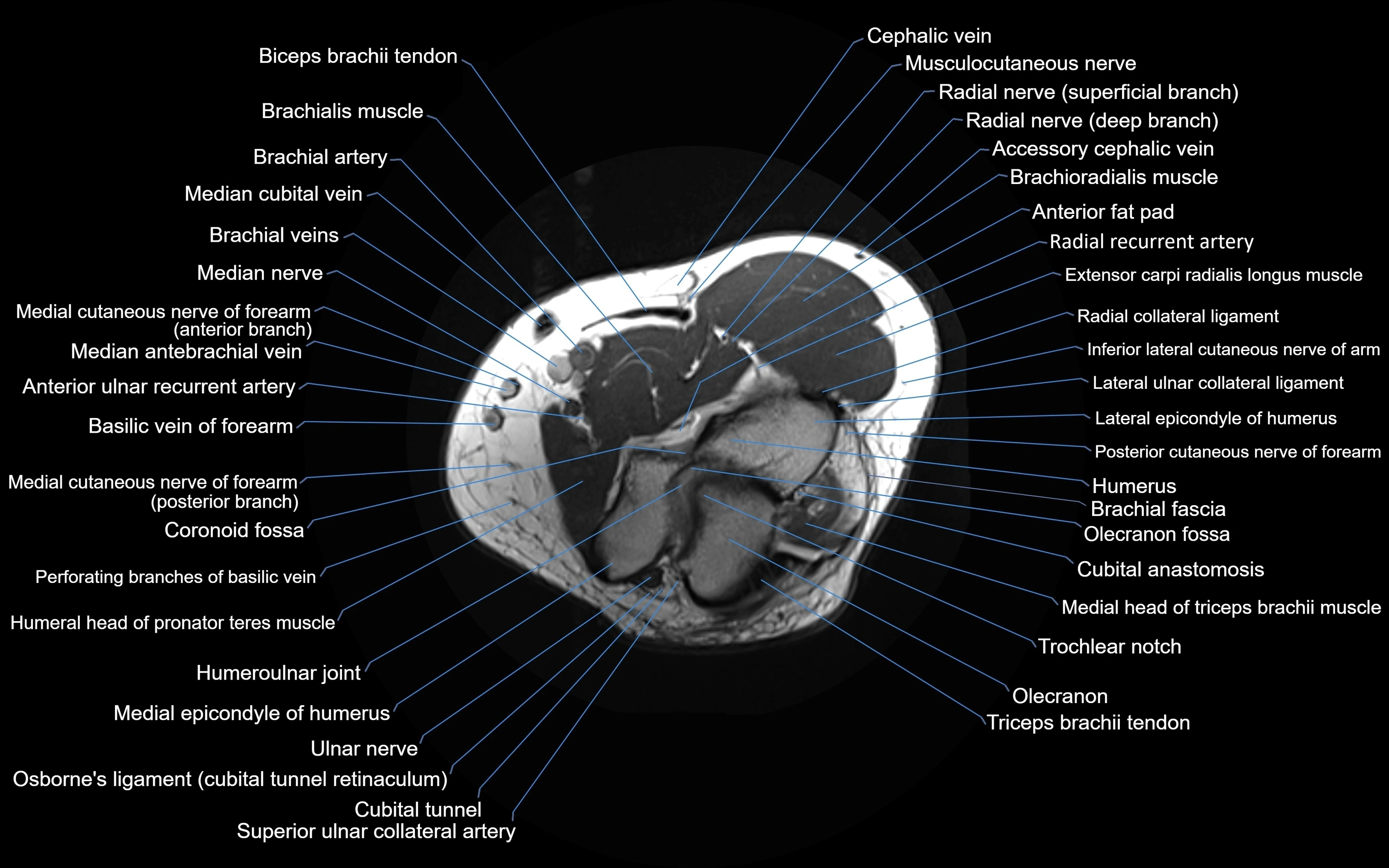
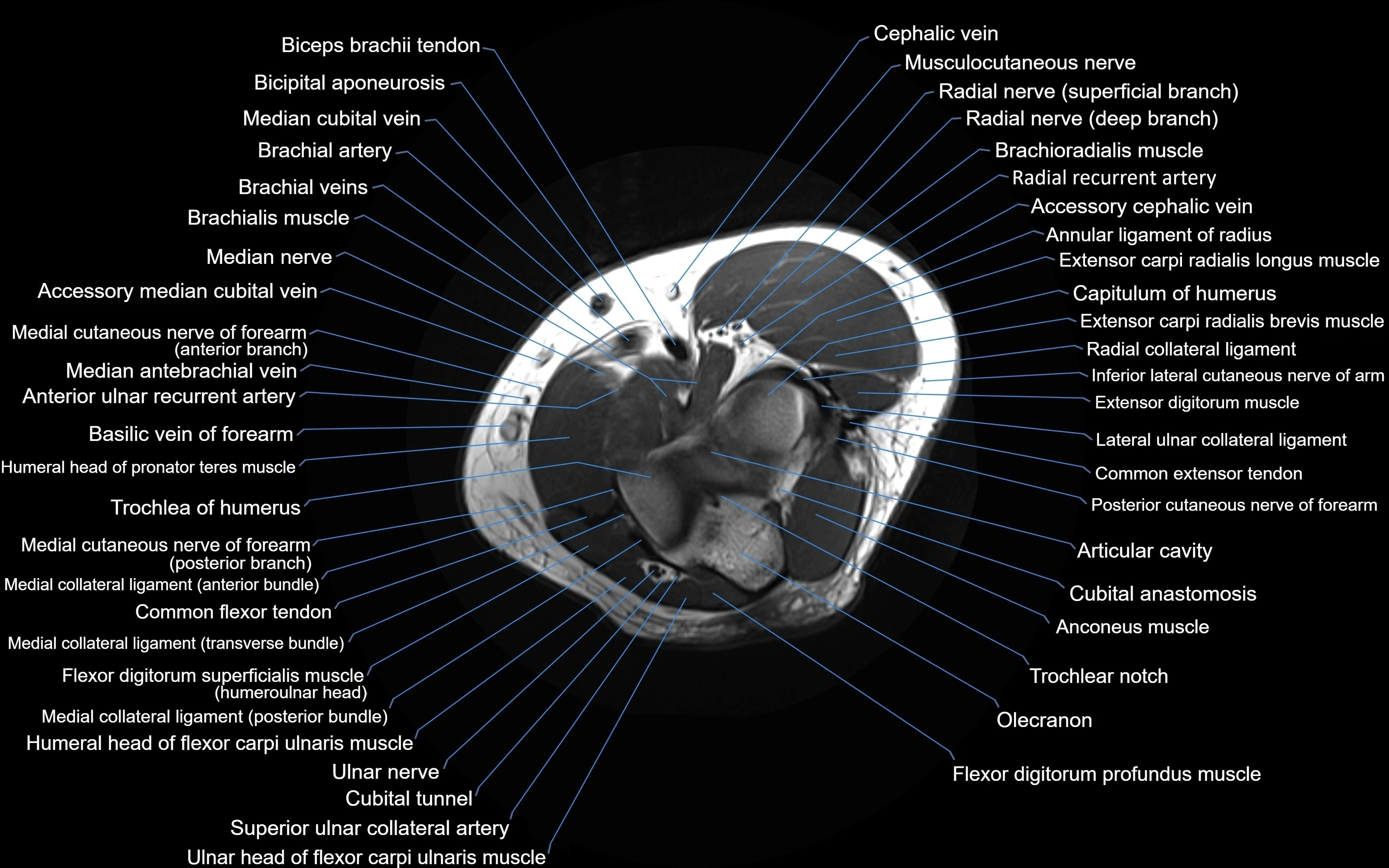
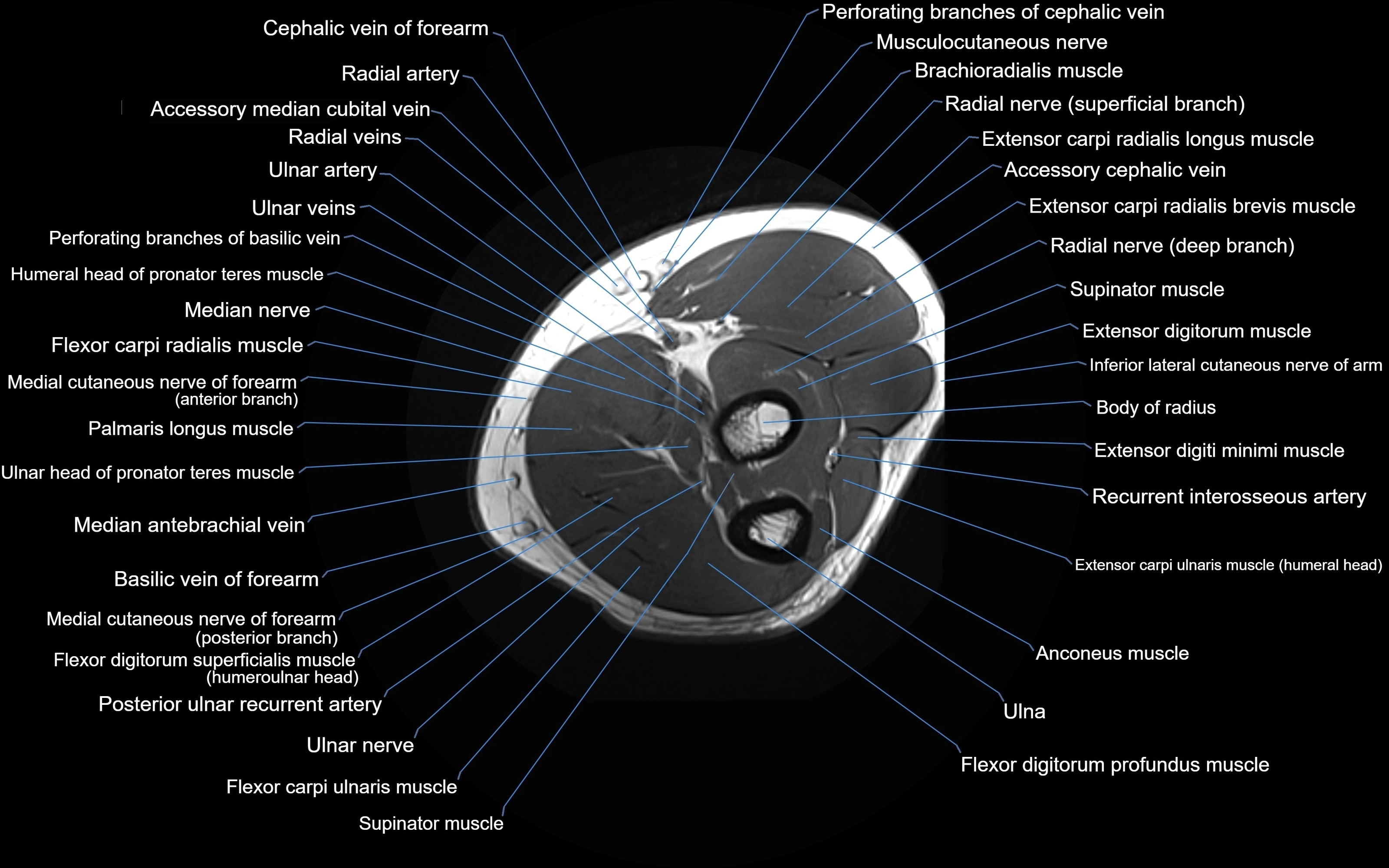
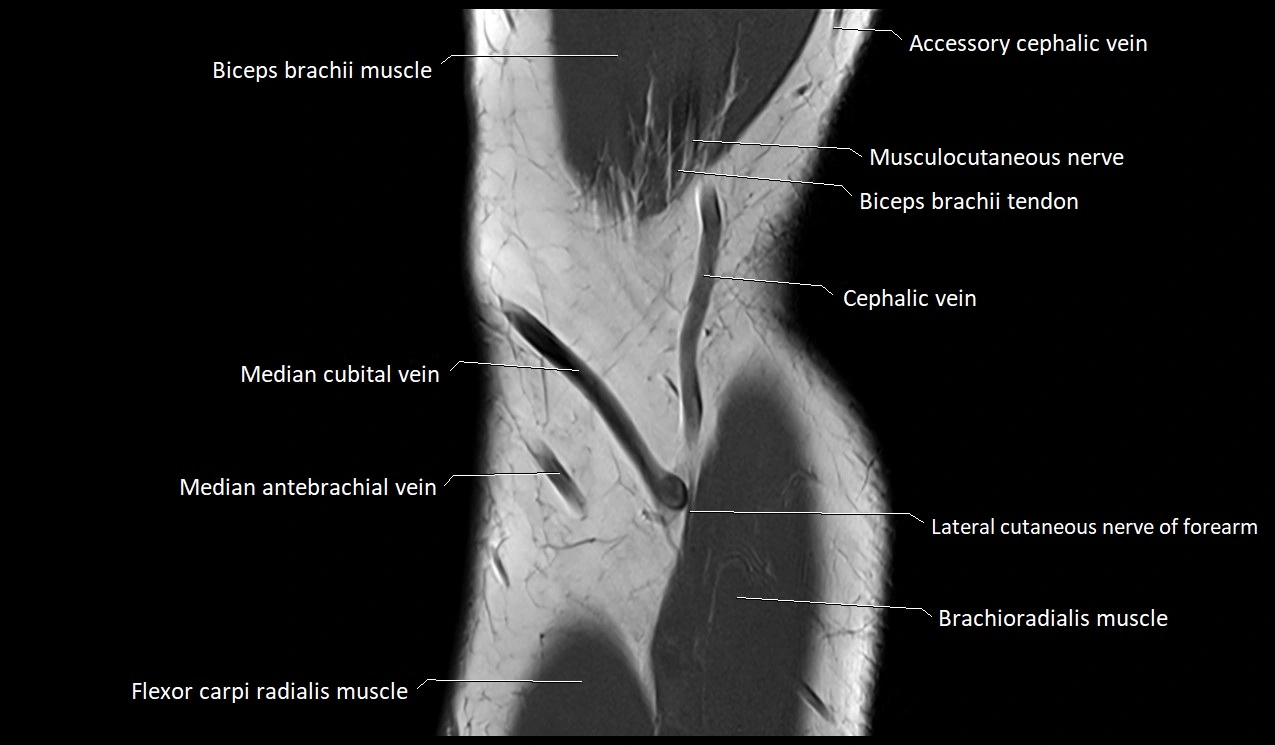
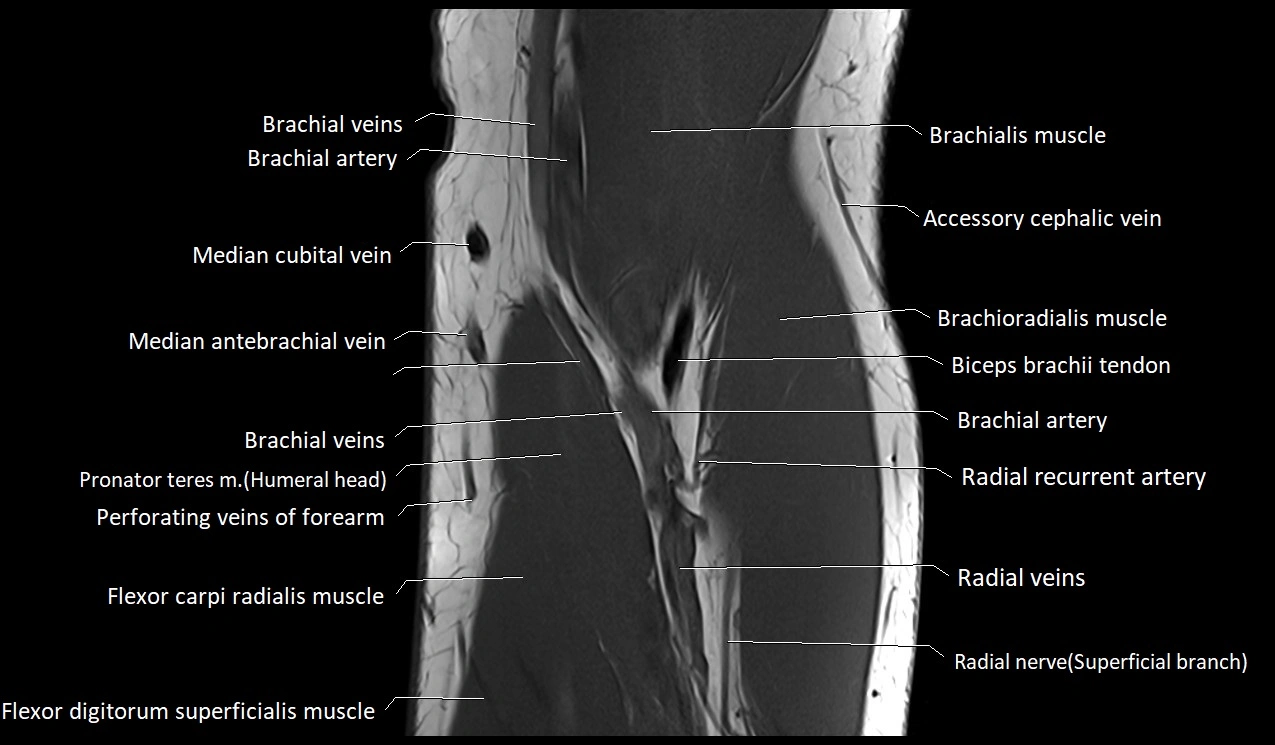
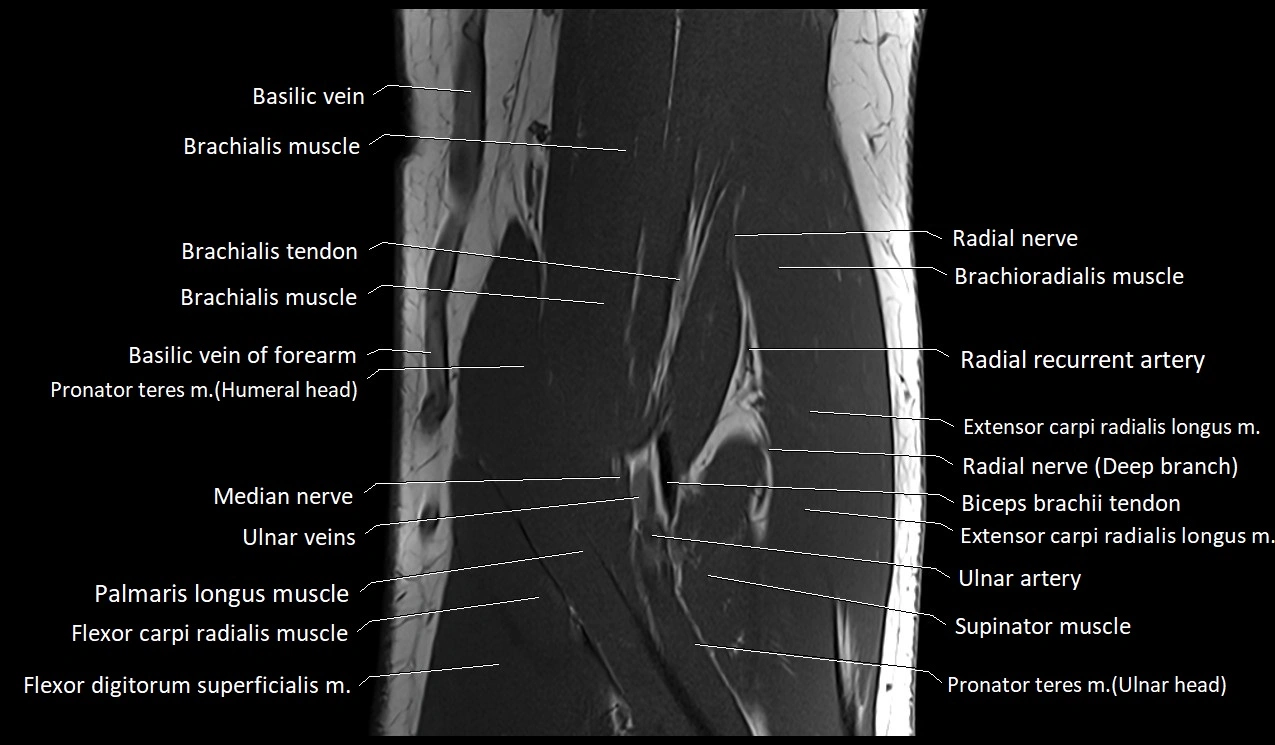
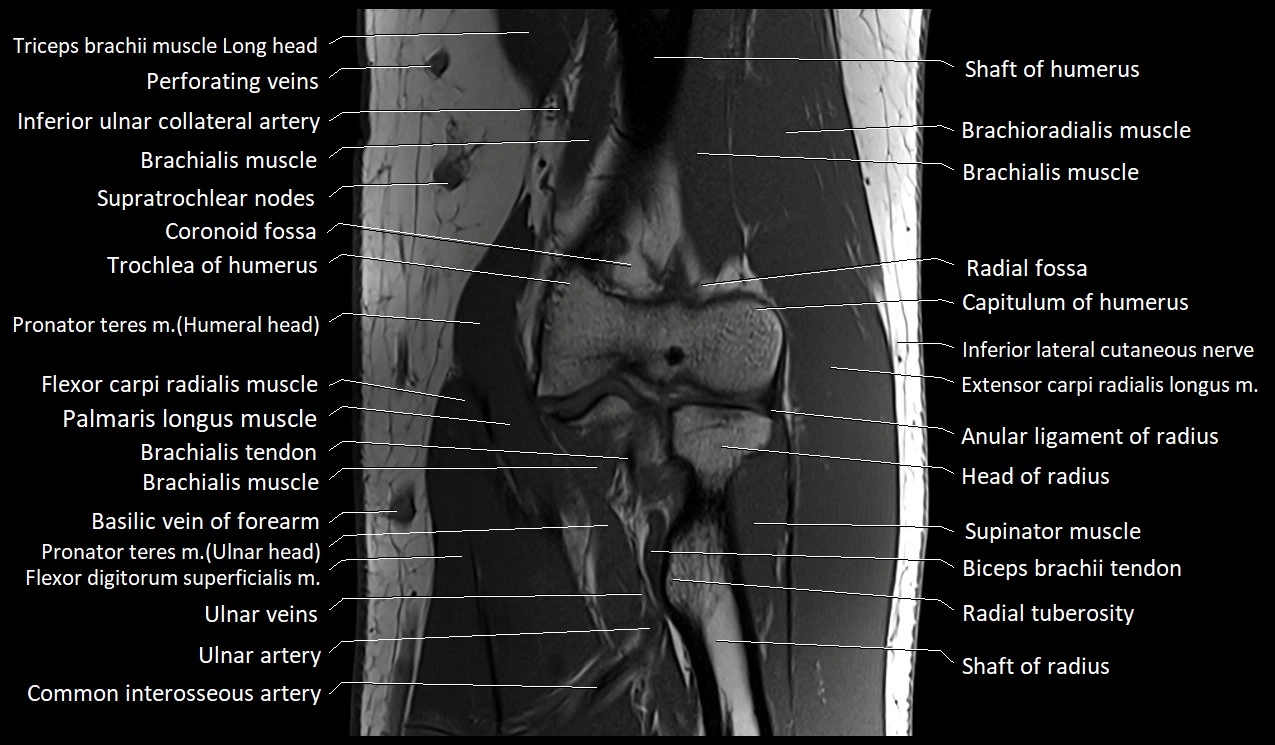
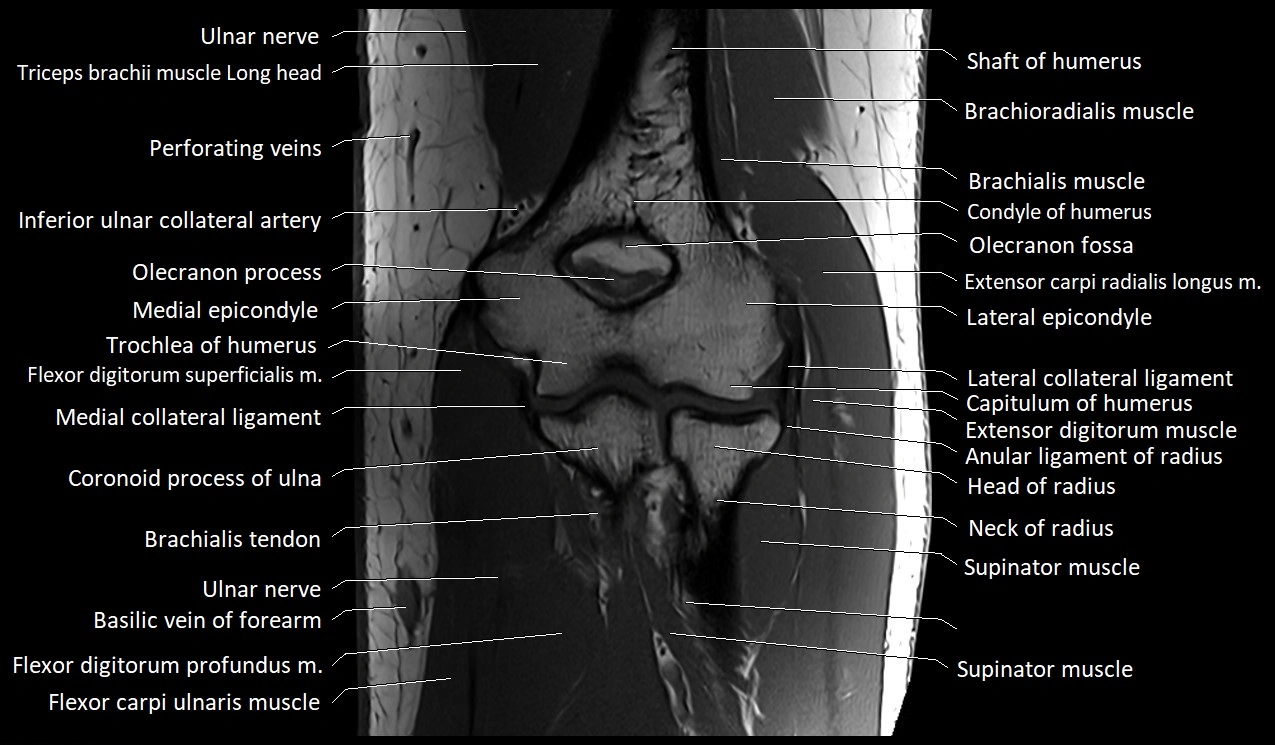
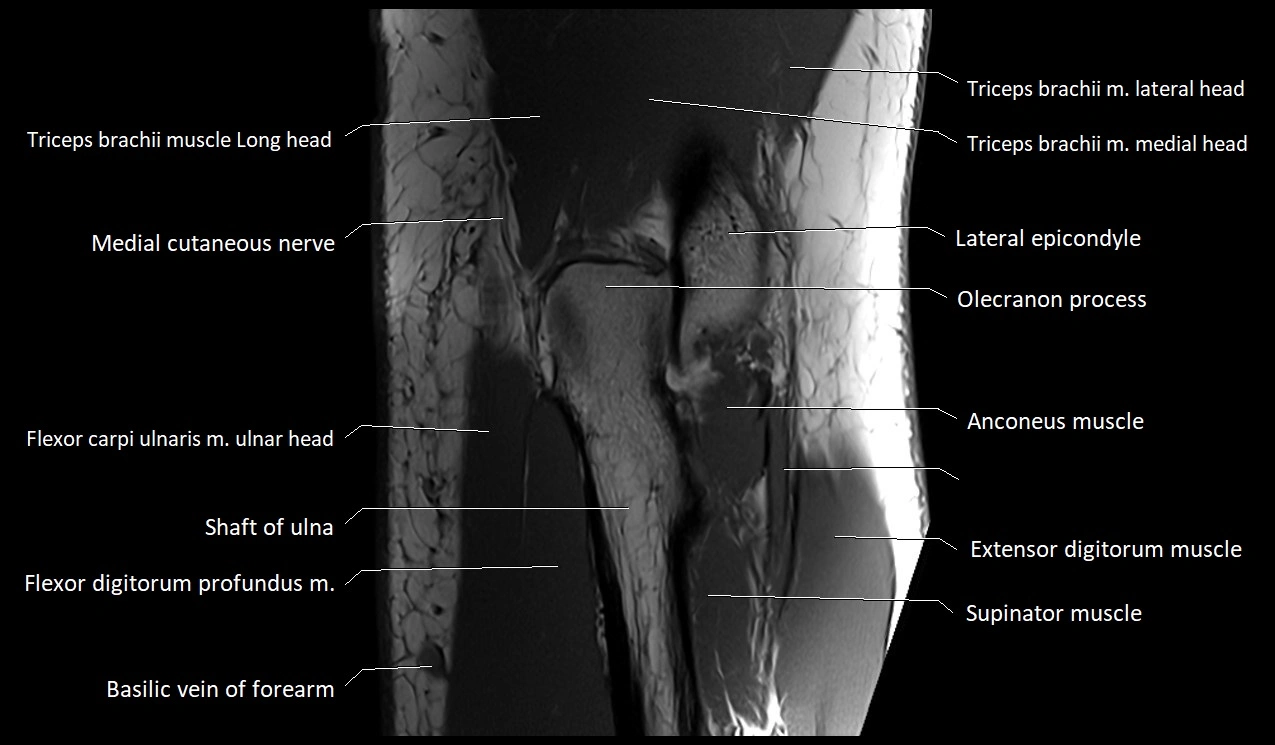
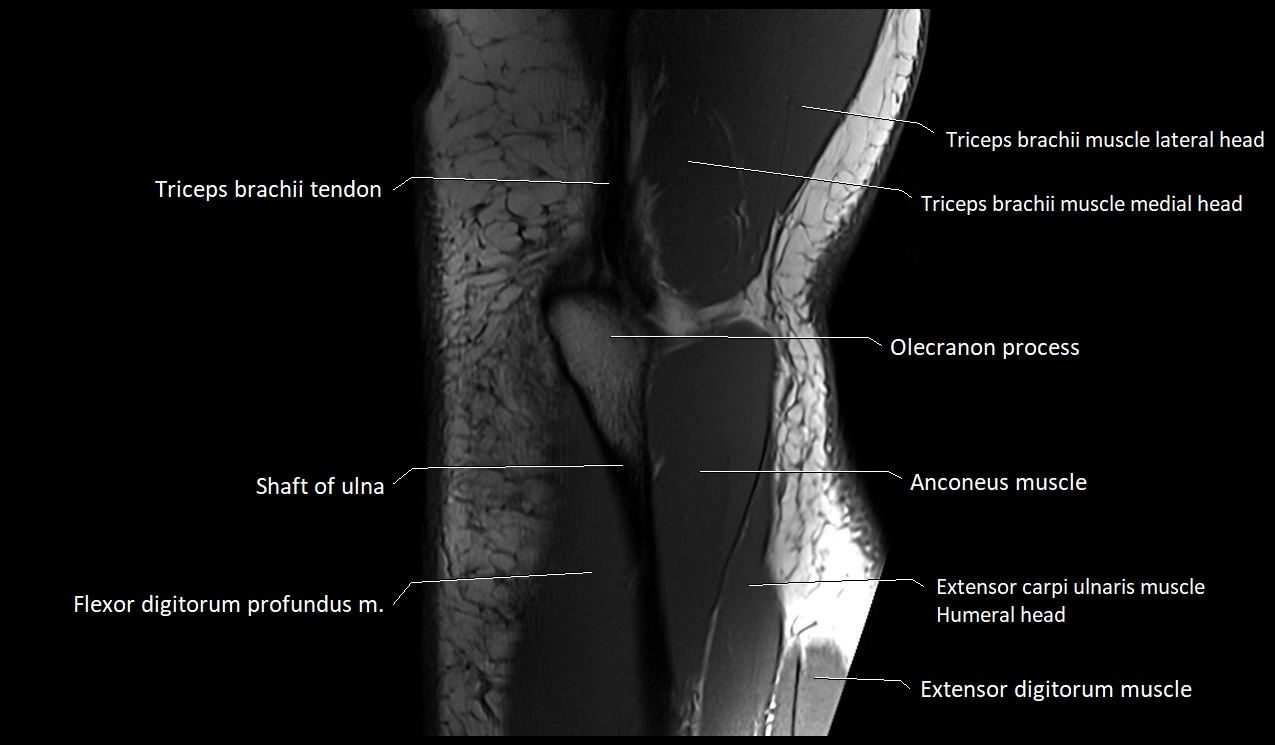
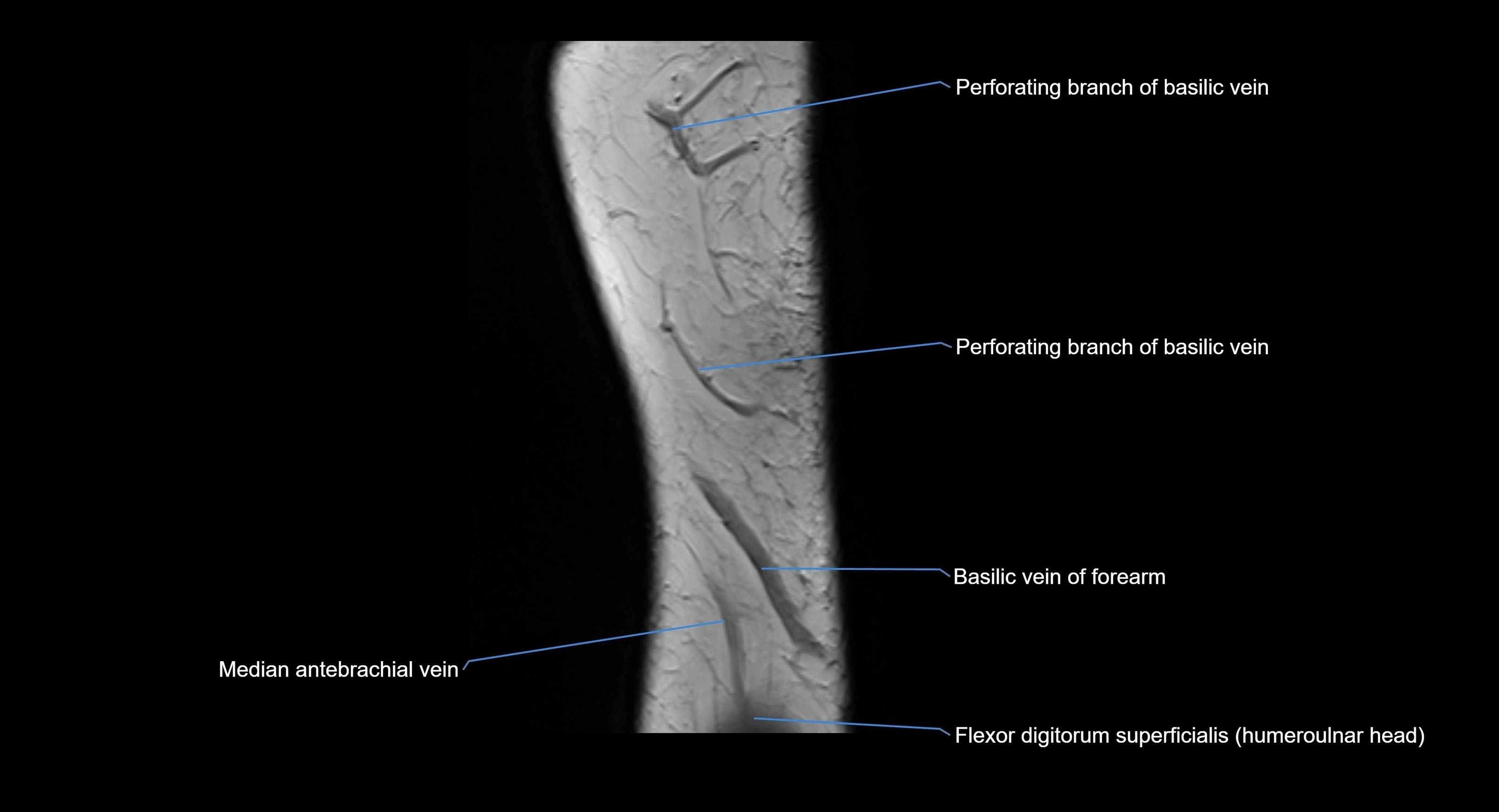
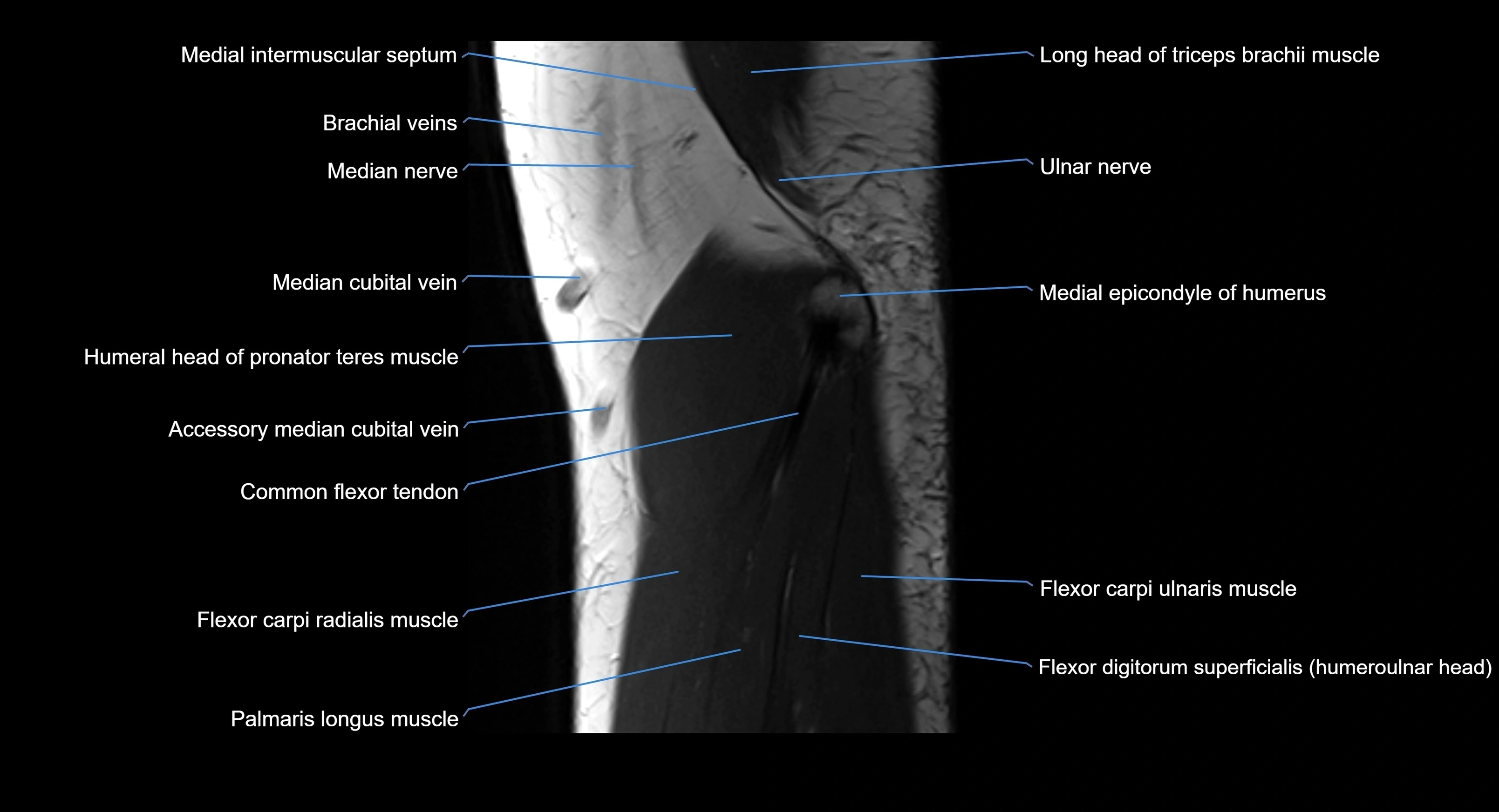
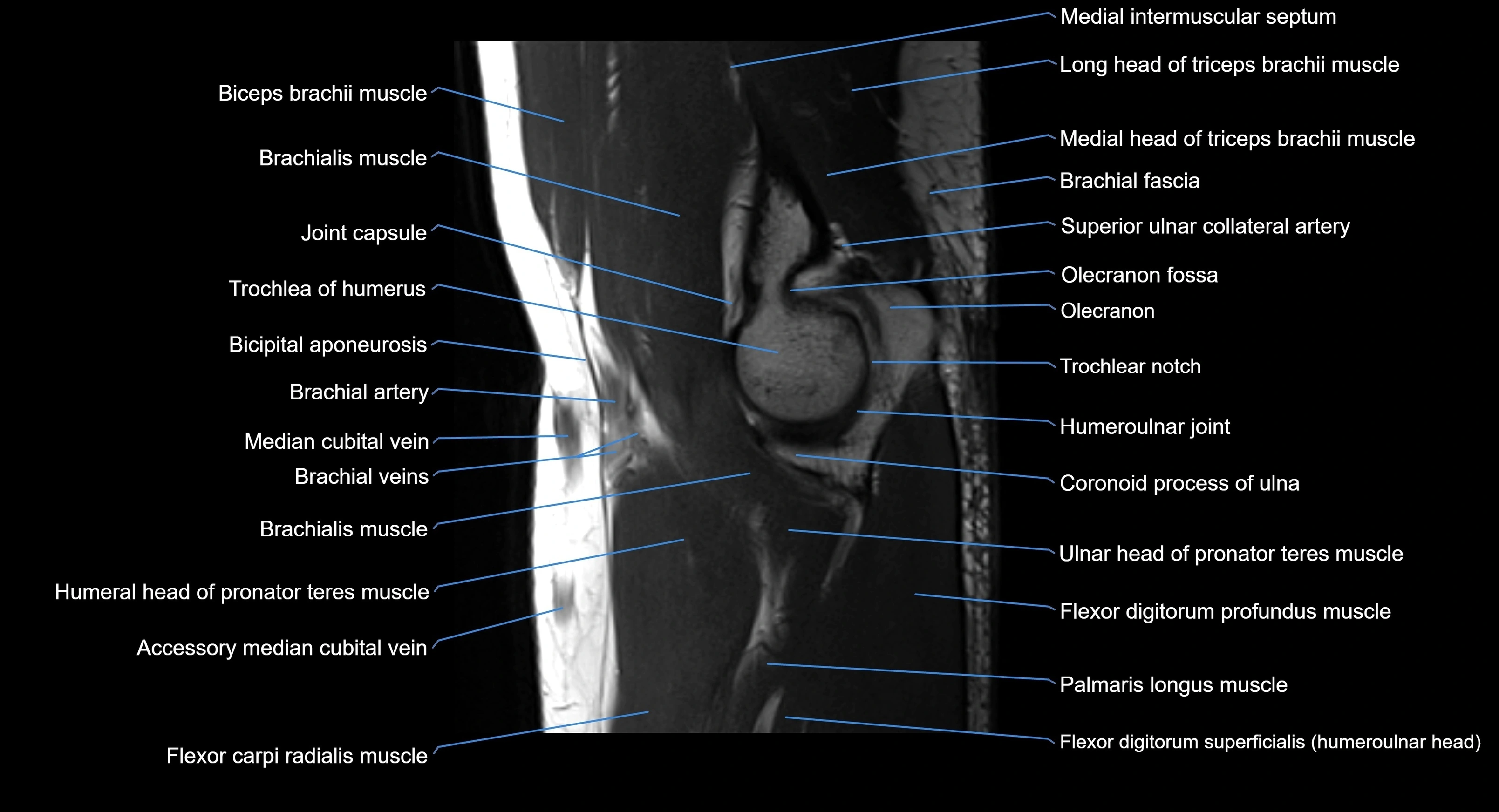
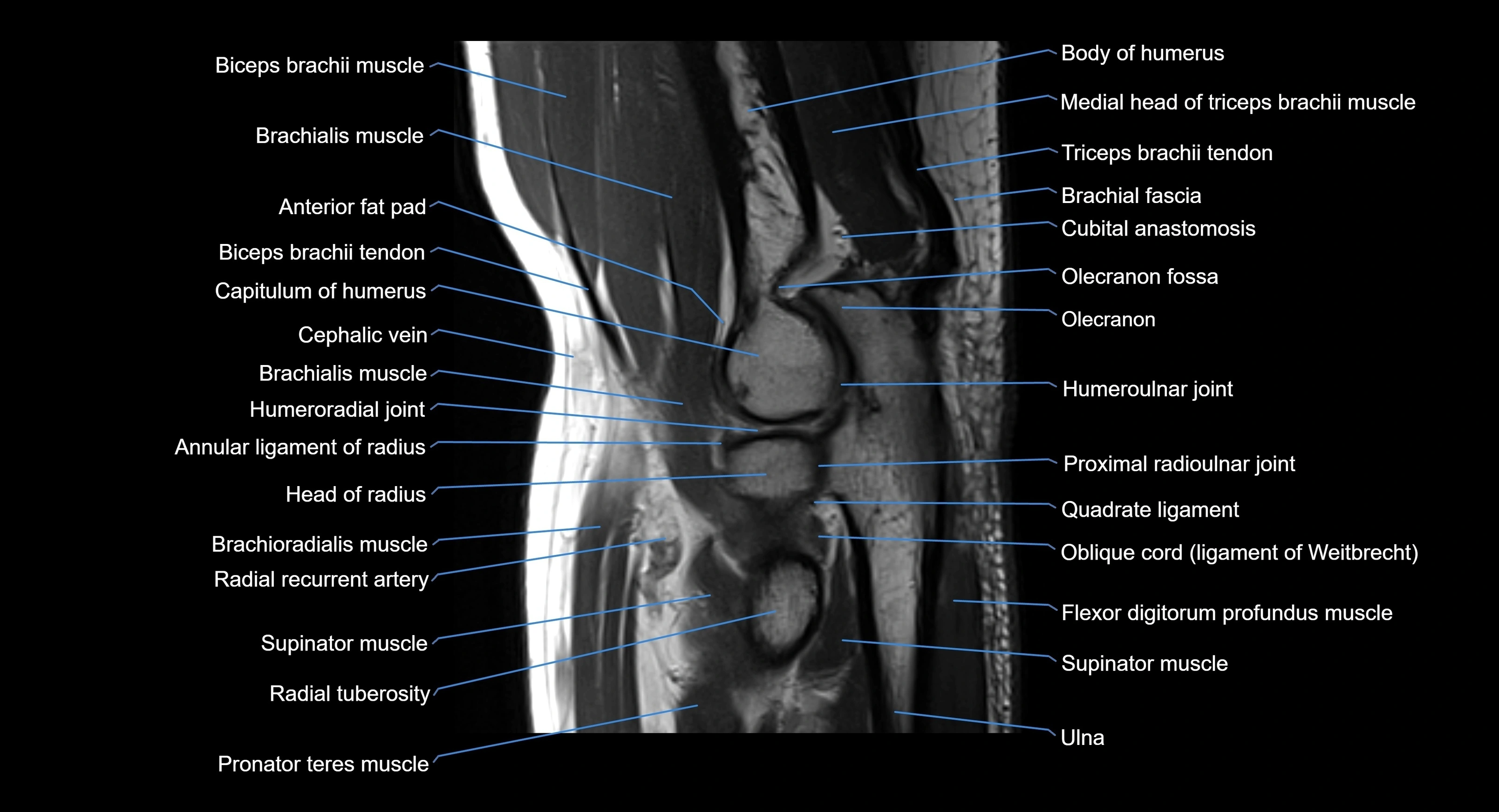
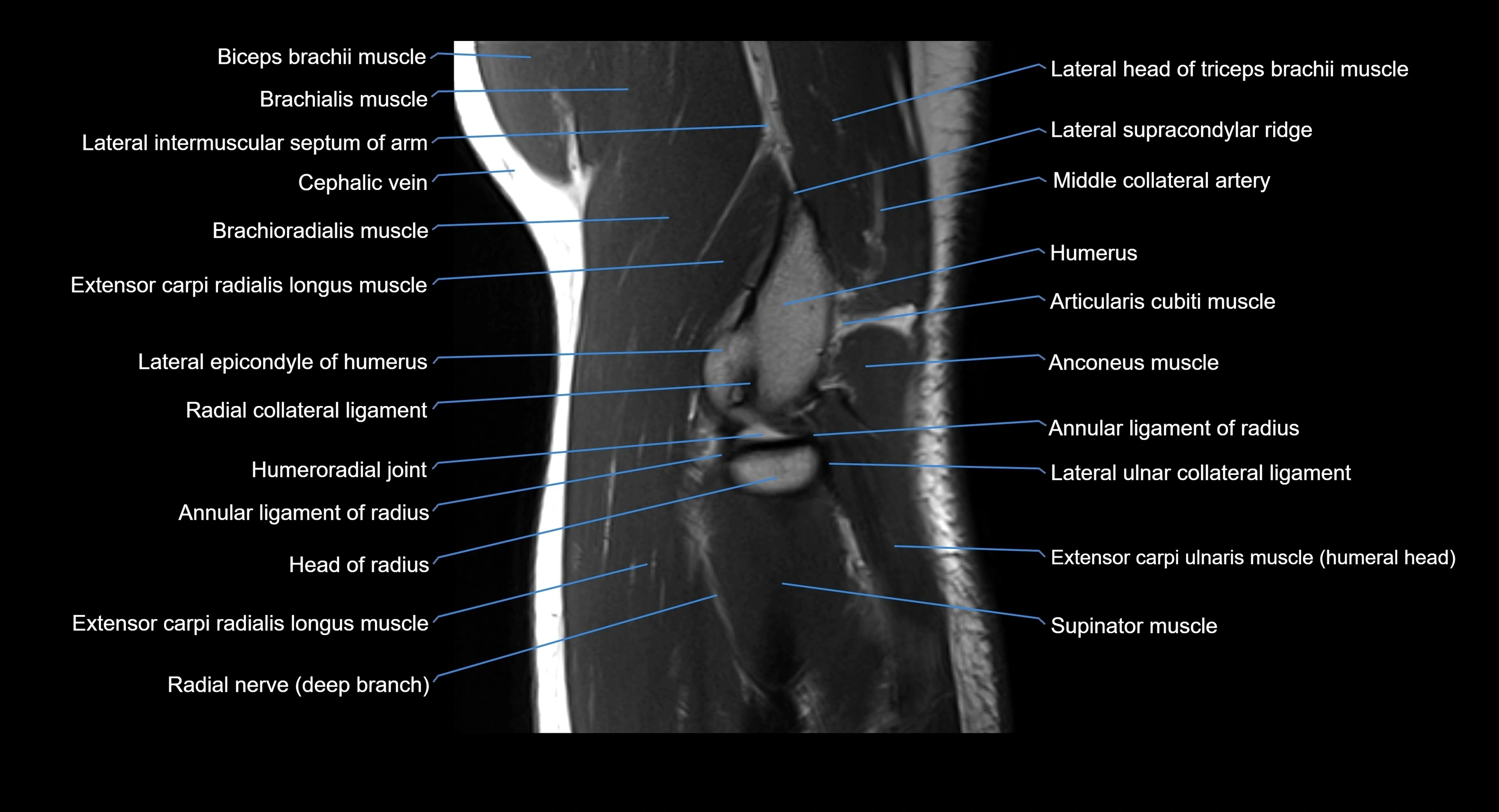
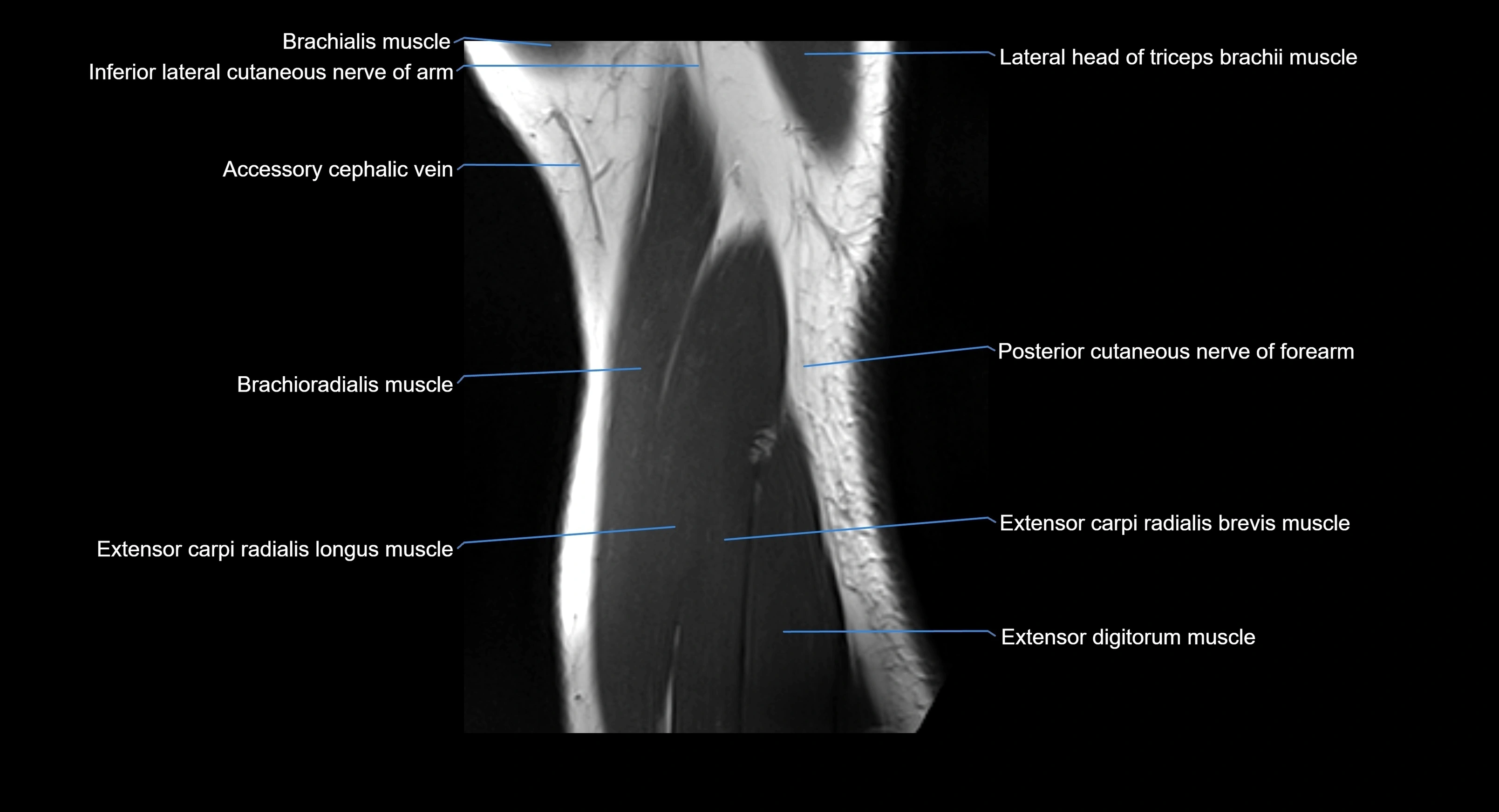
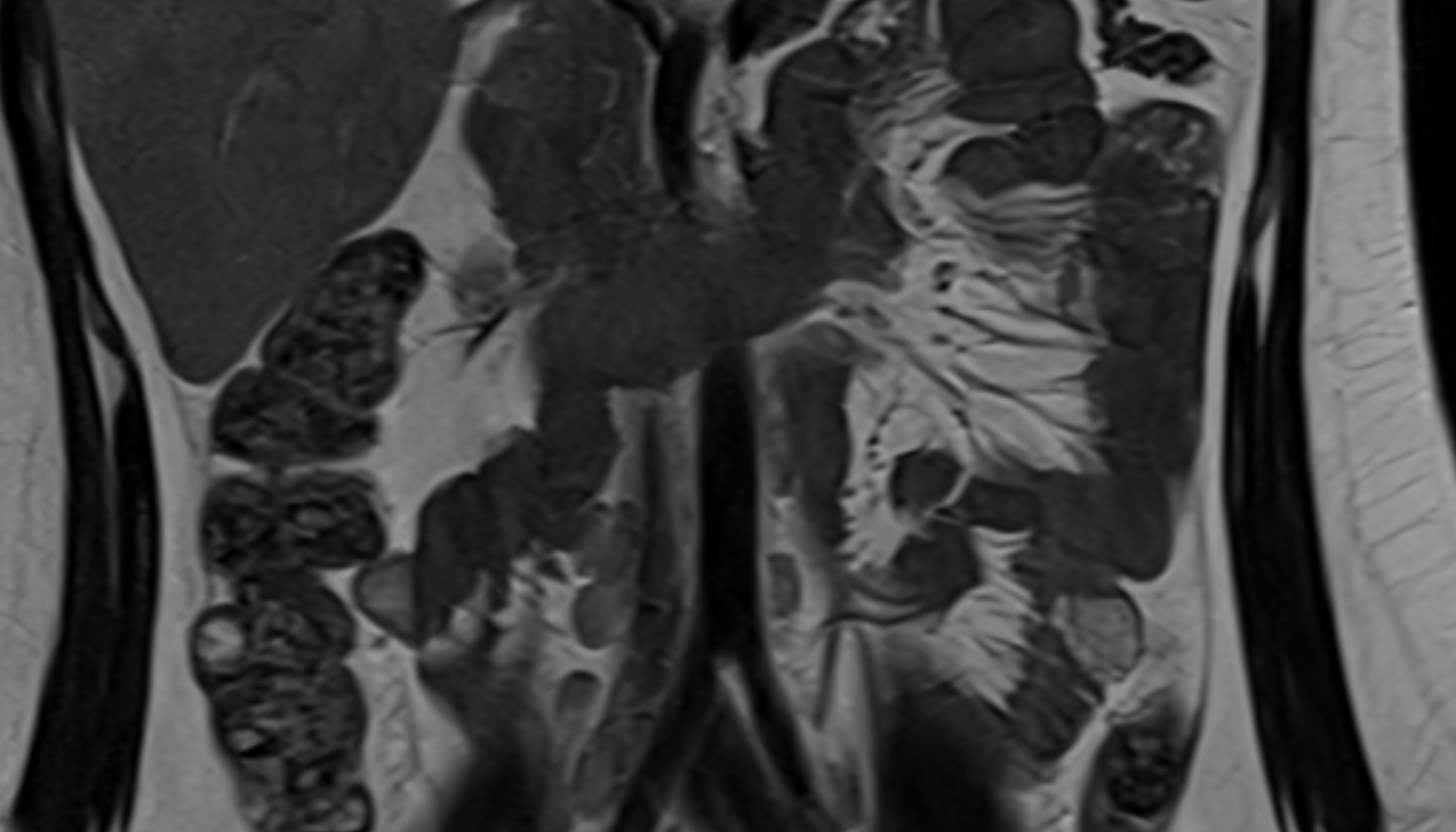
MRI image

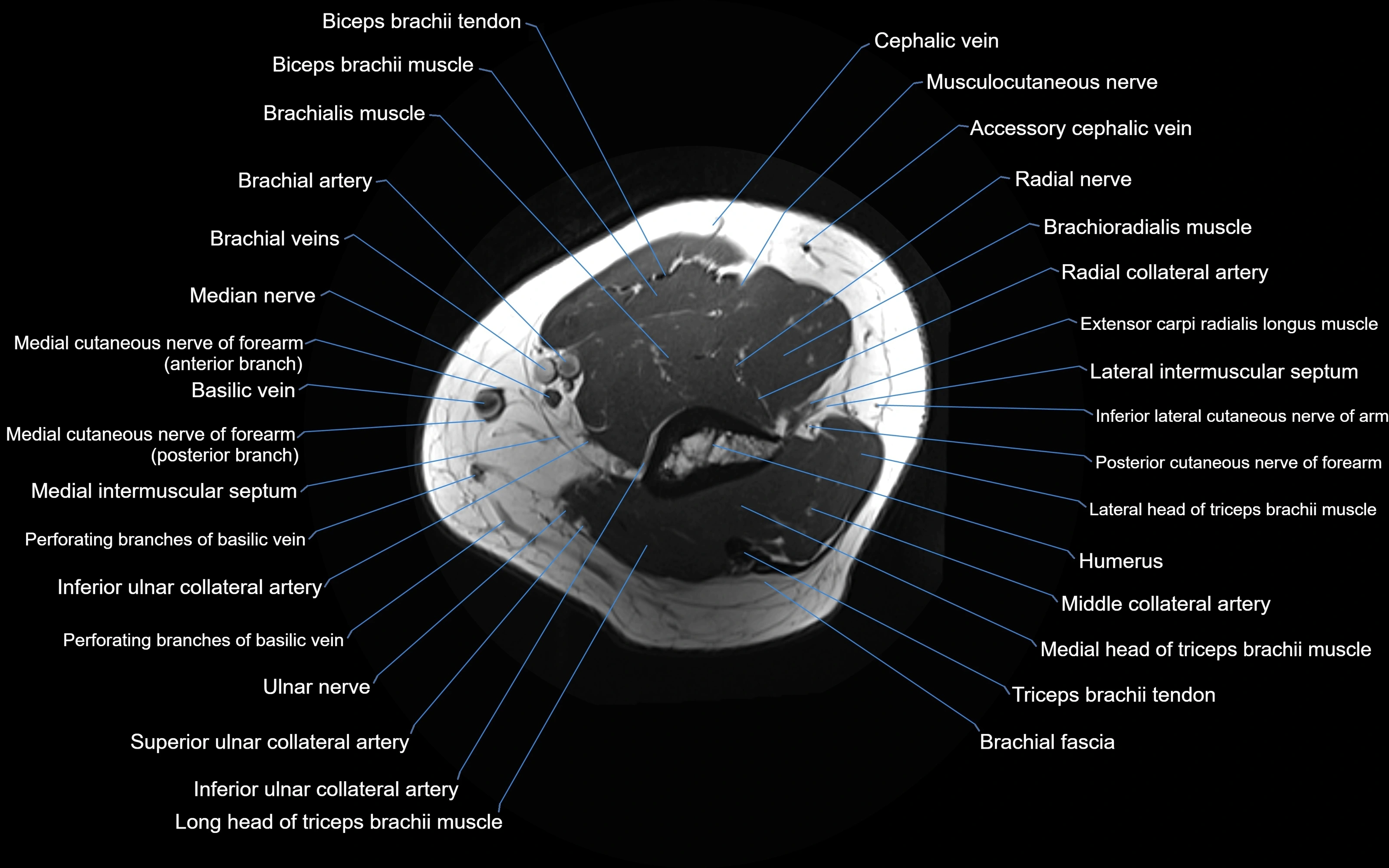
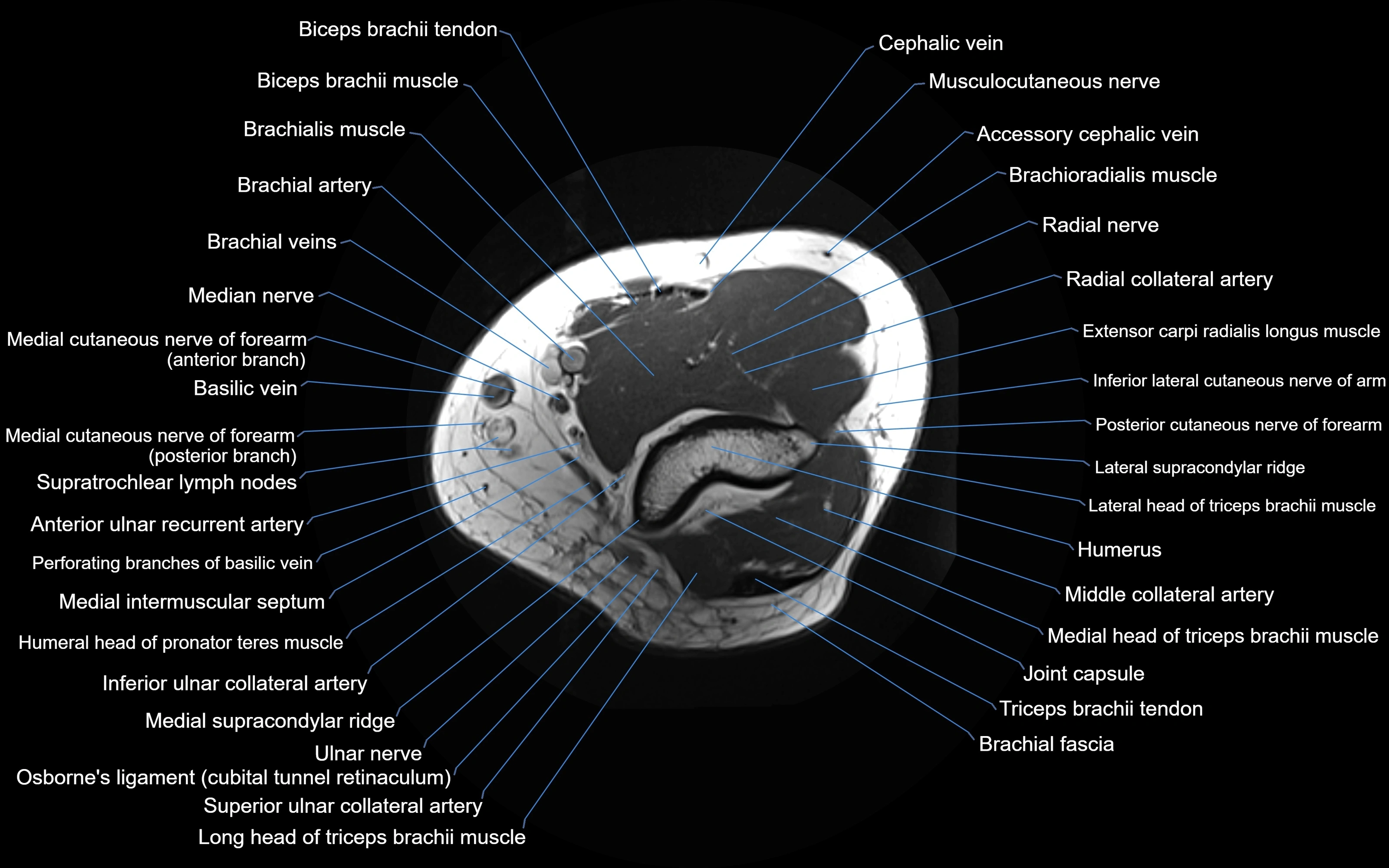
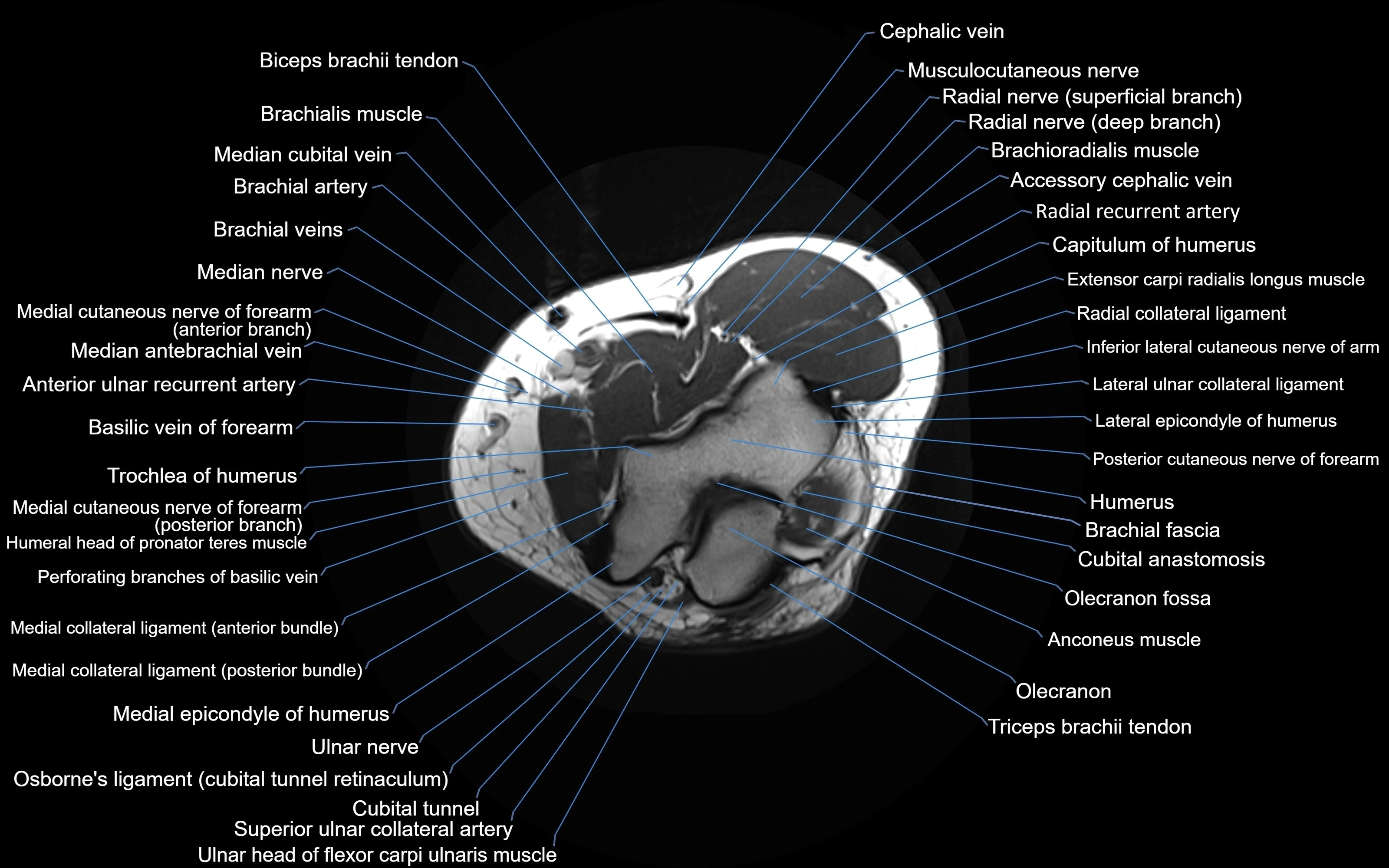
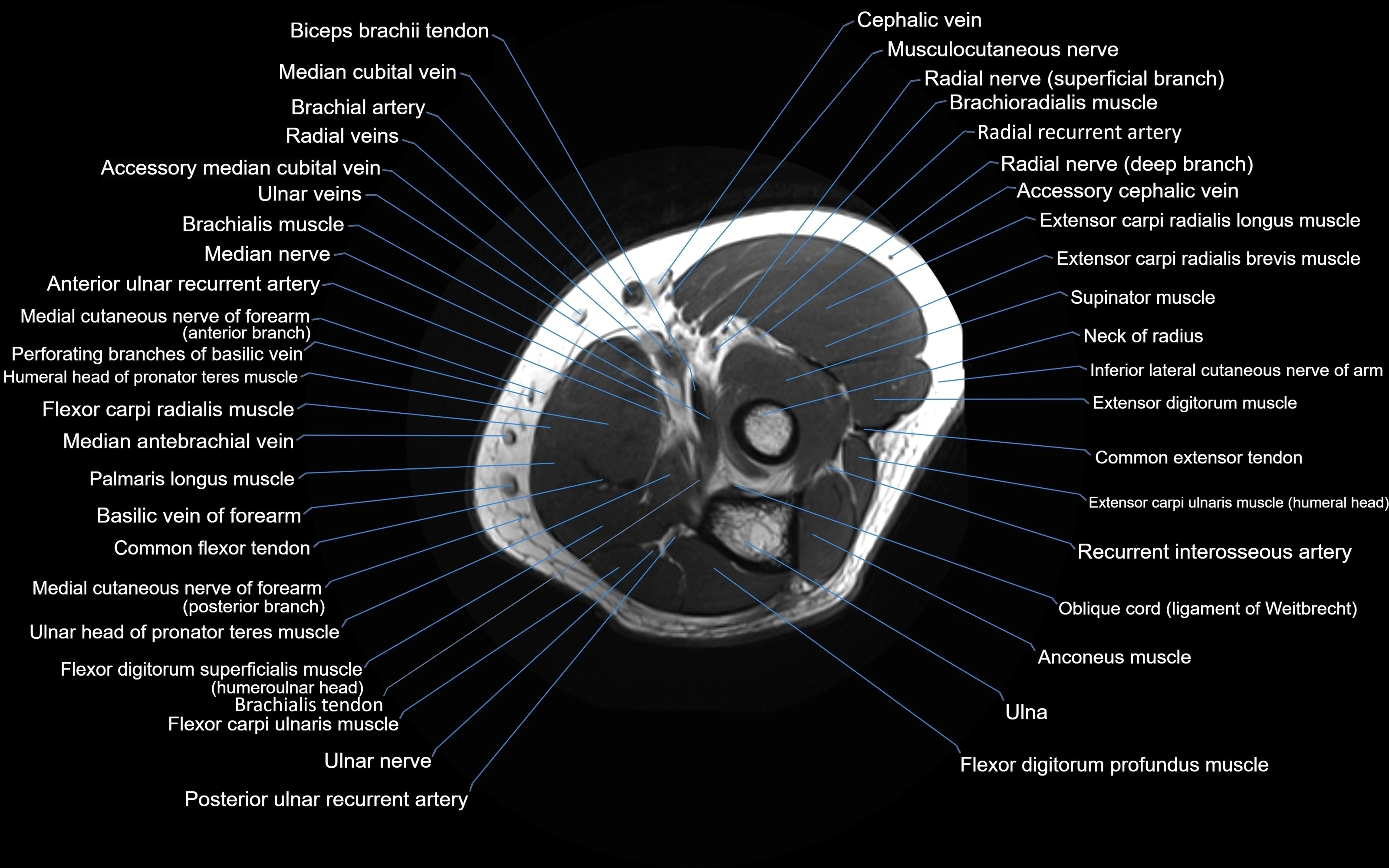
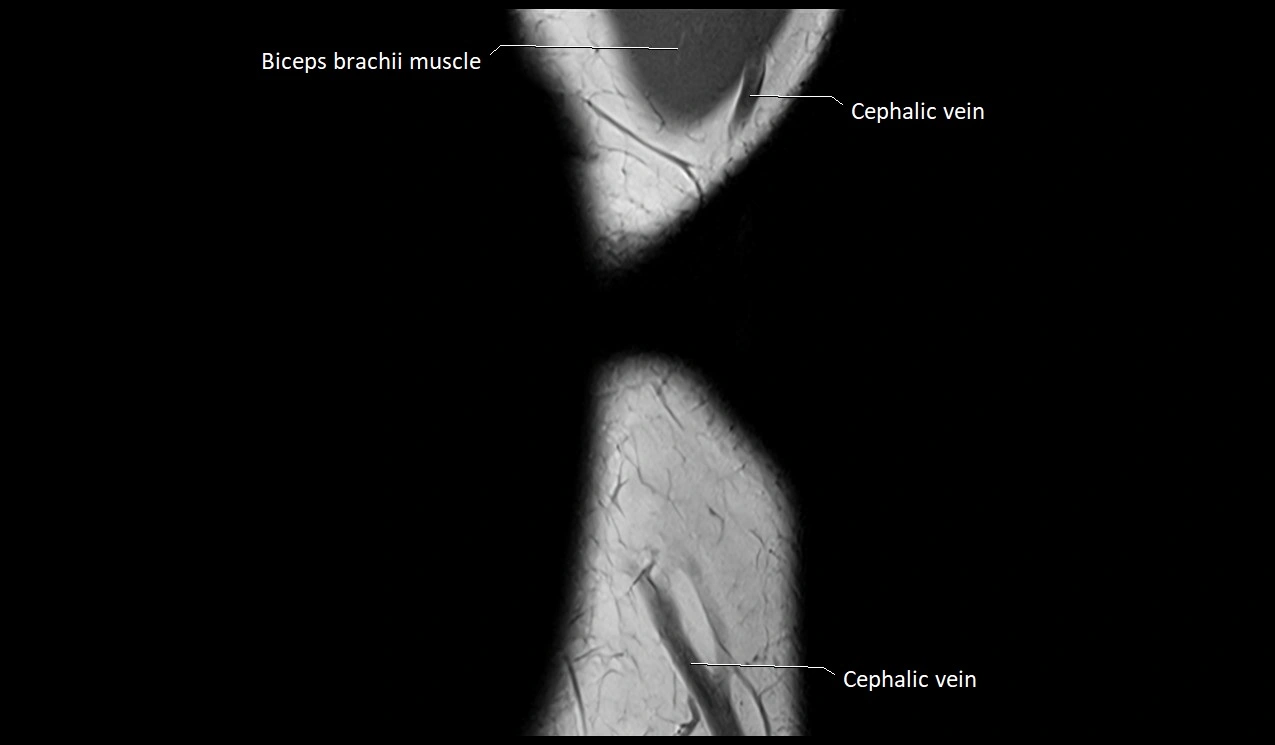
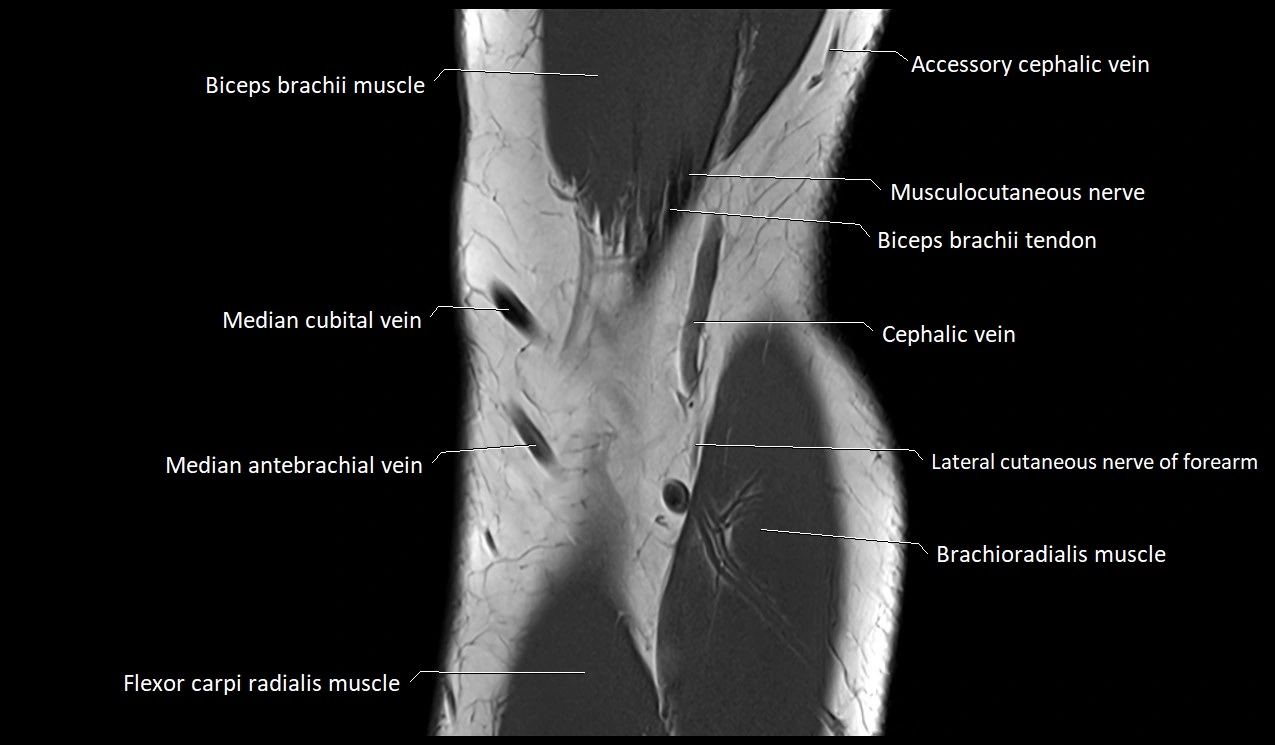
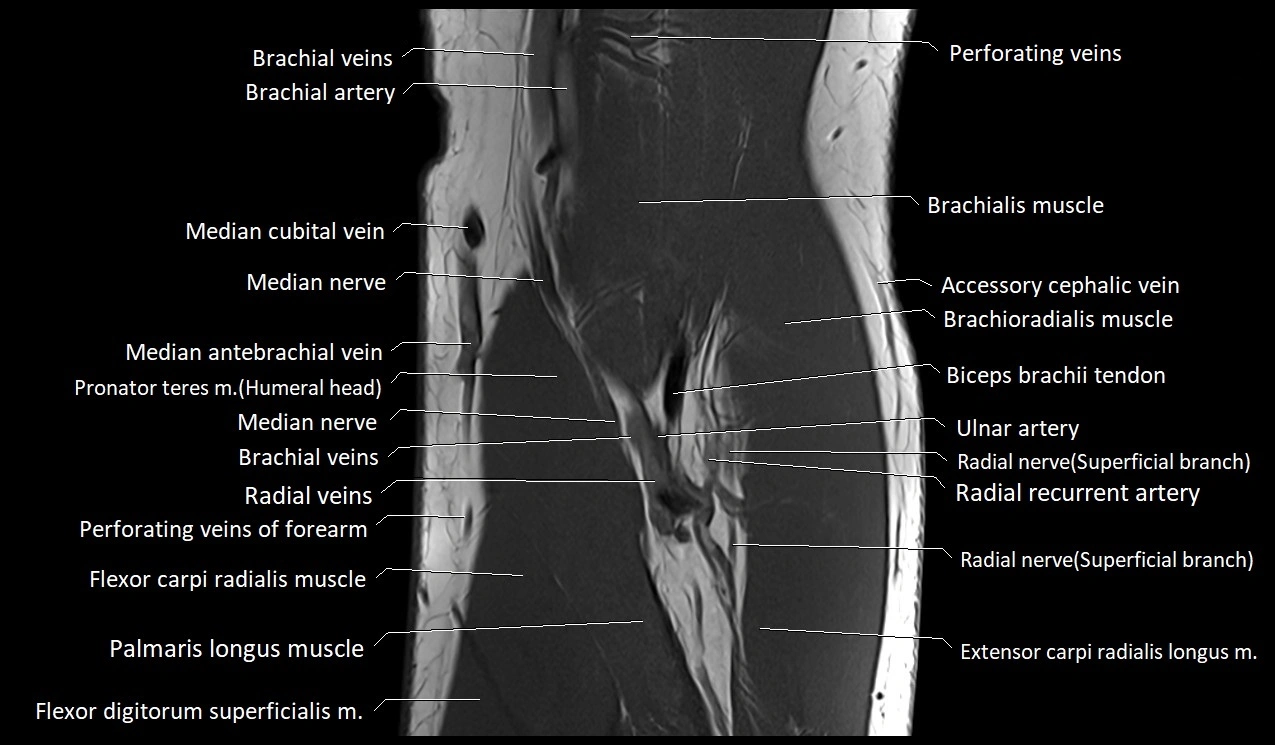
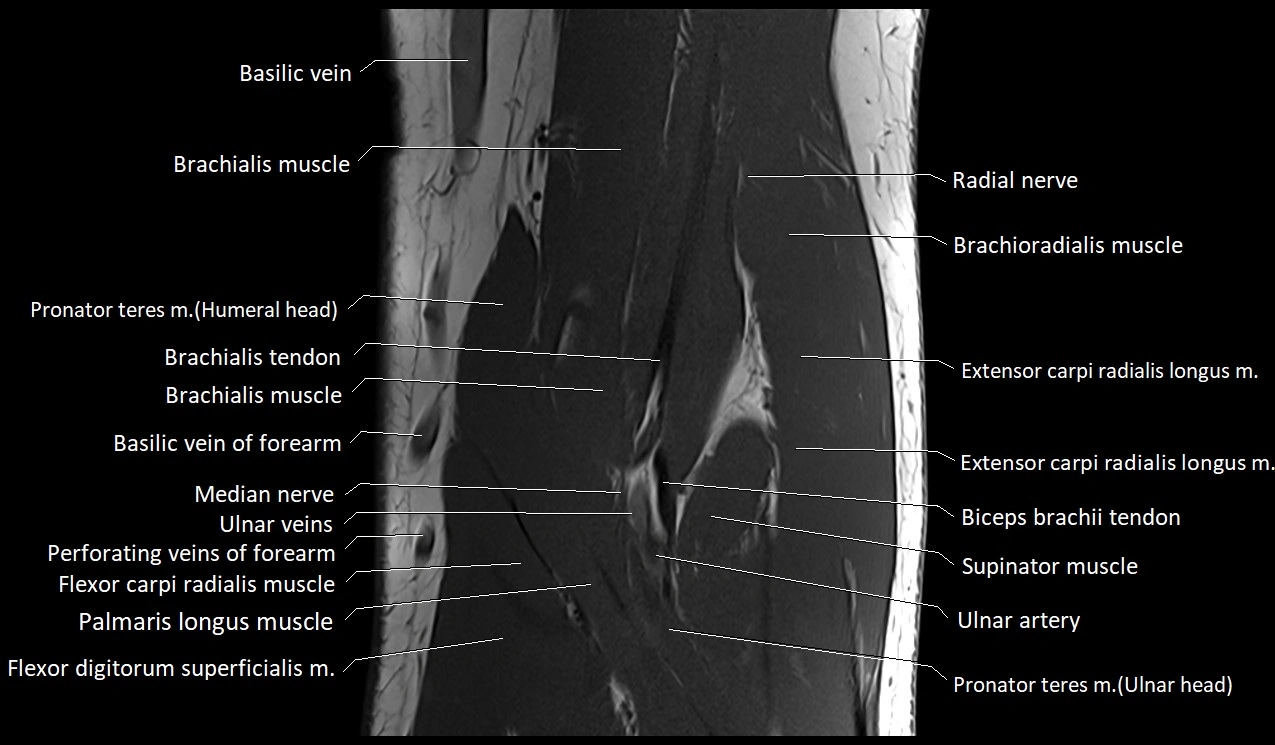
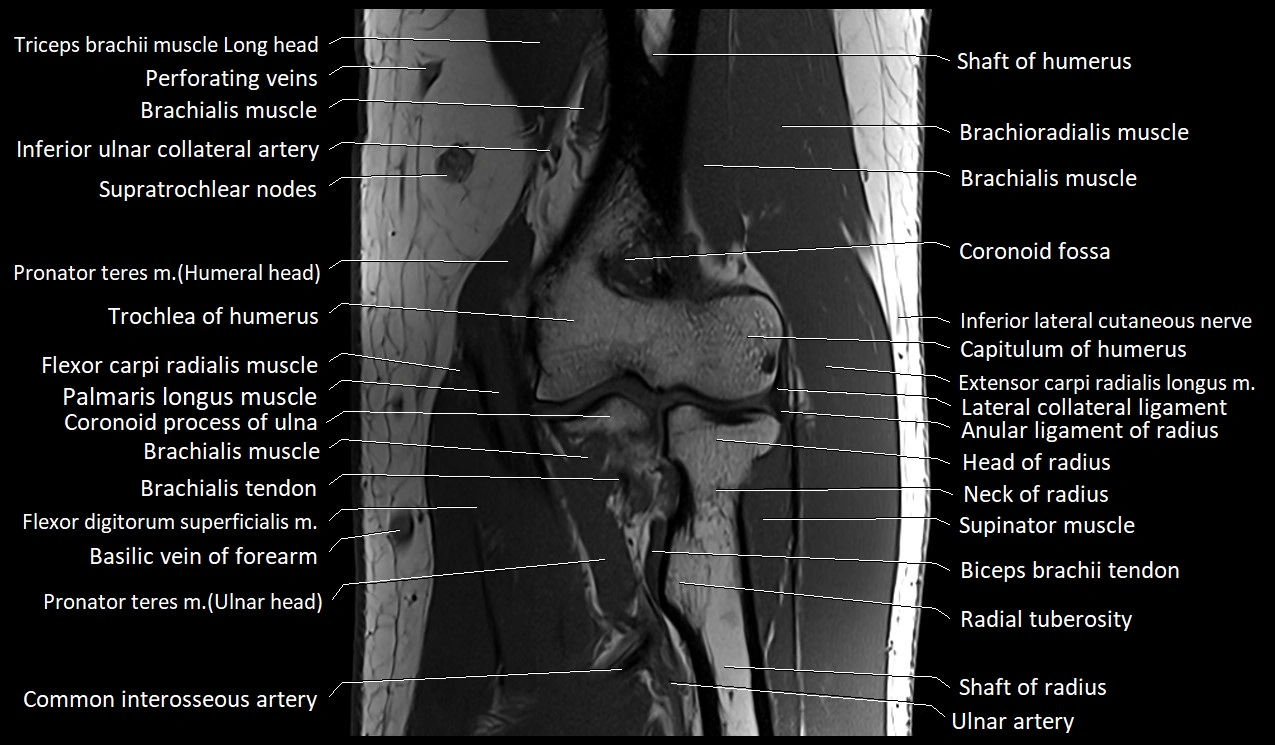
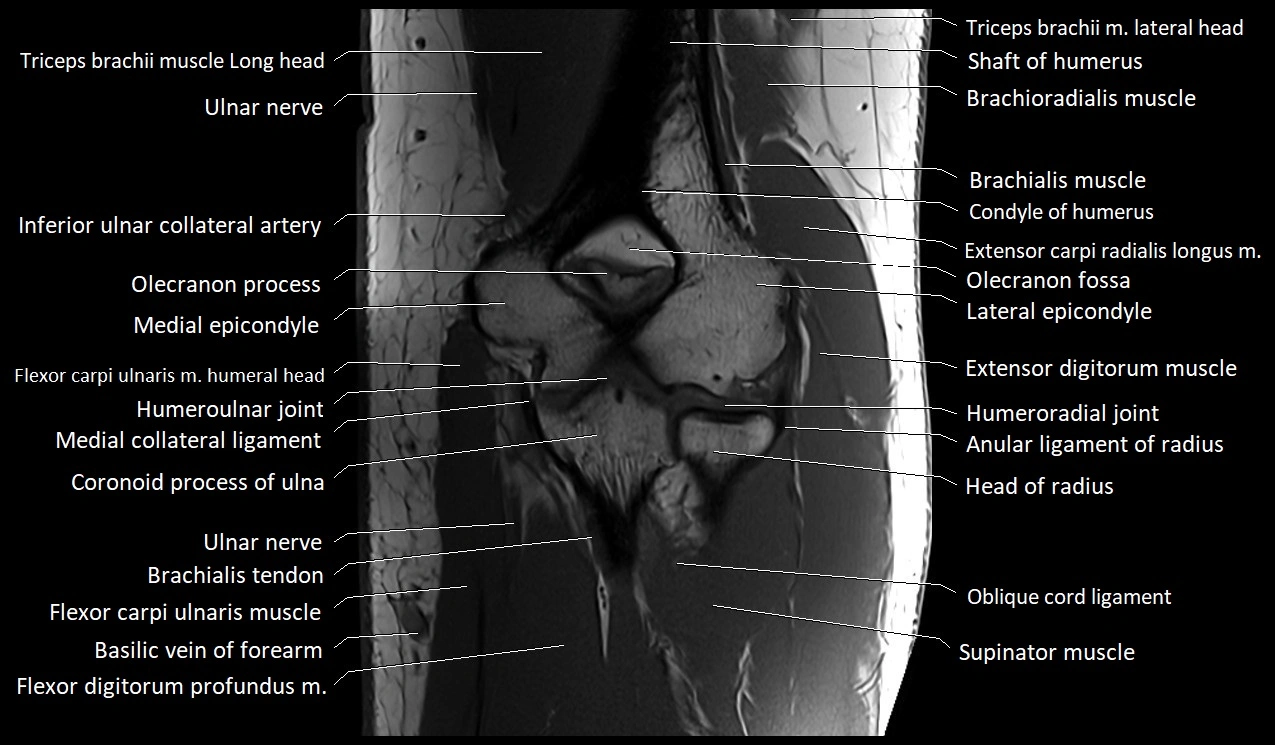
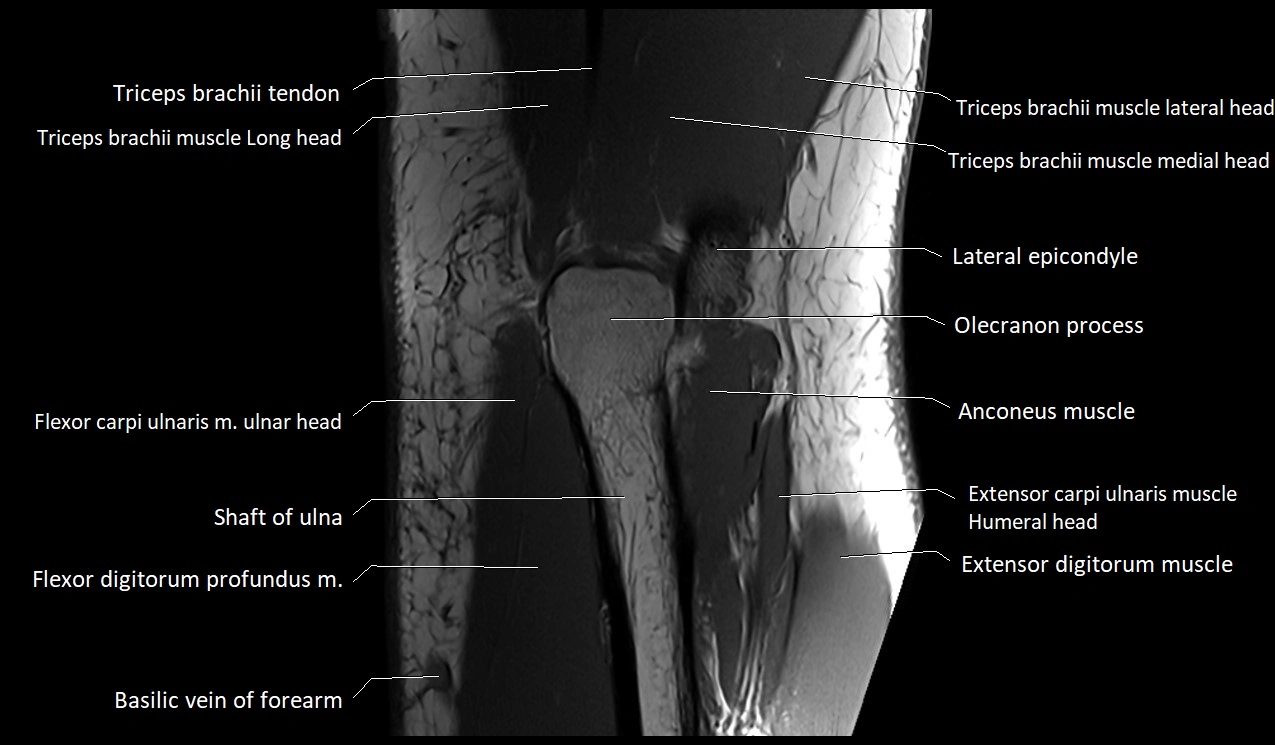
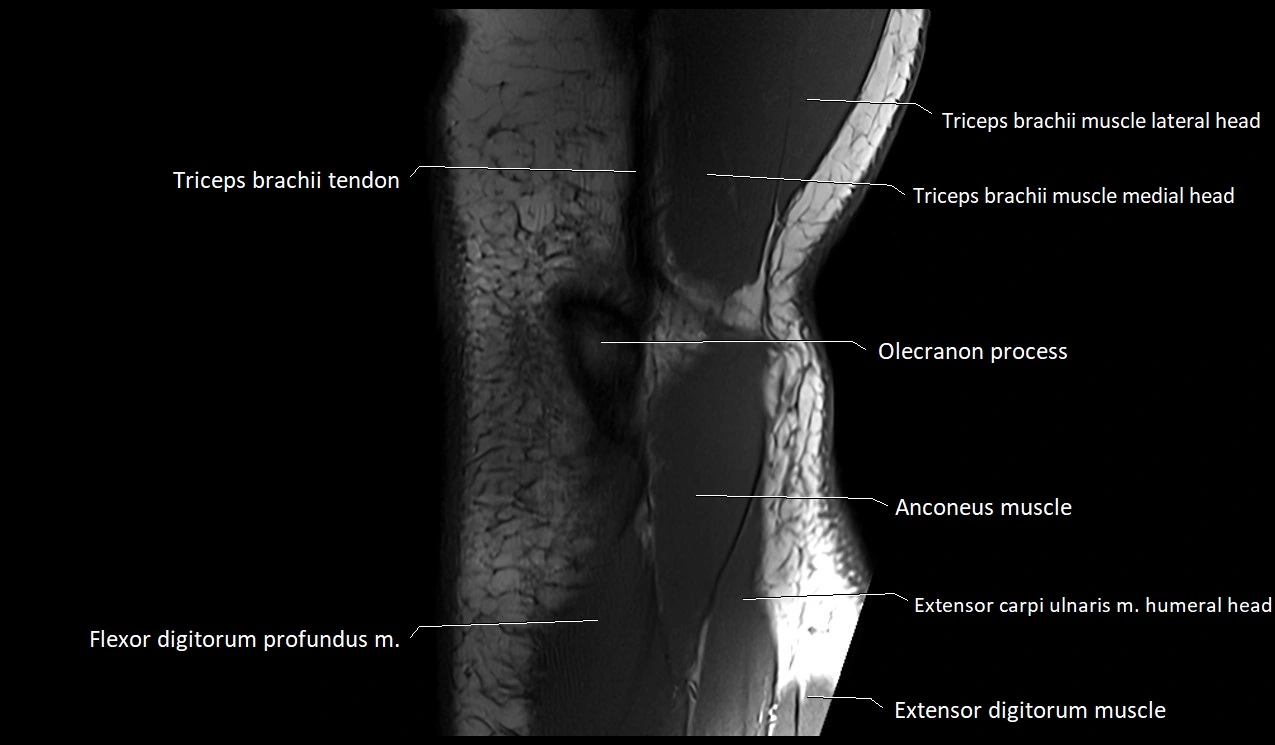
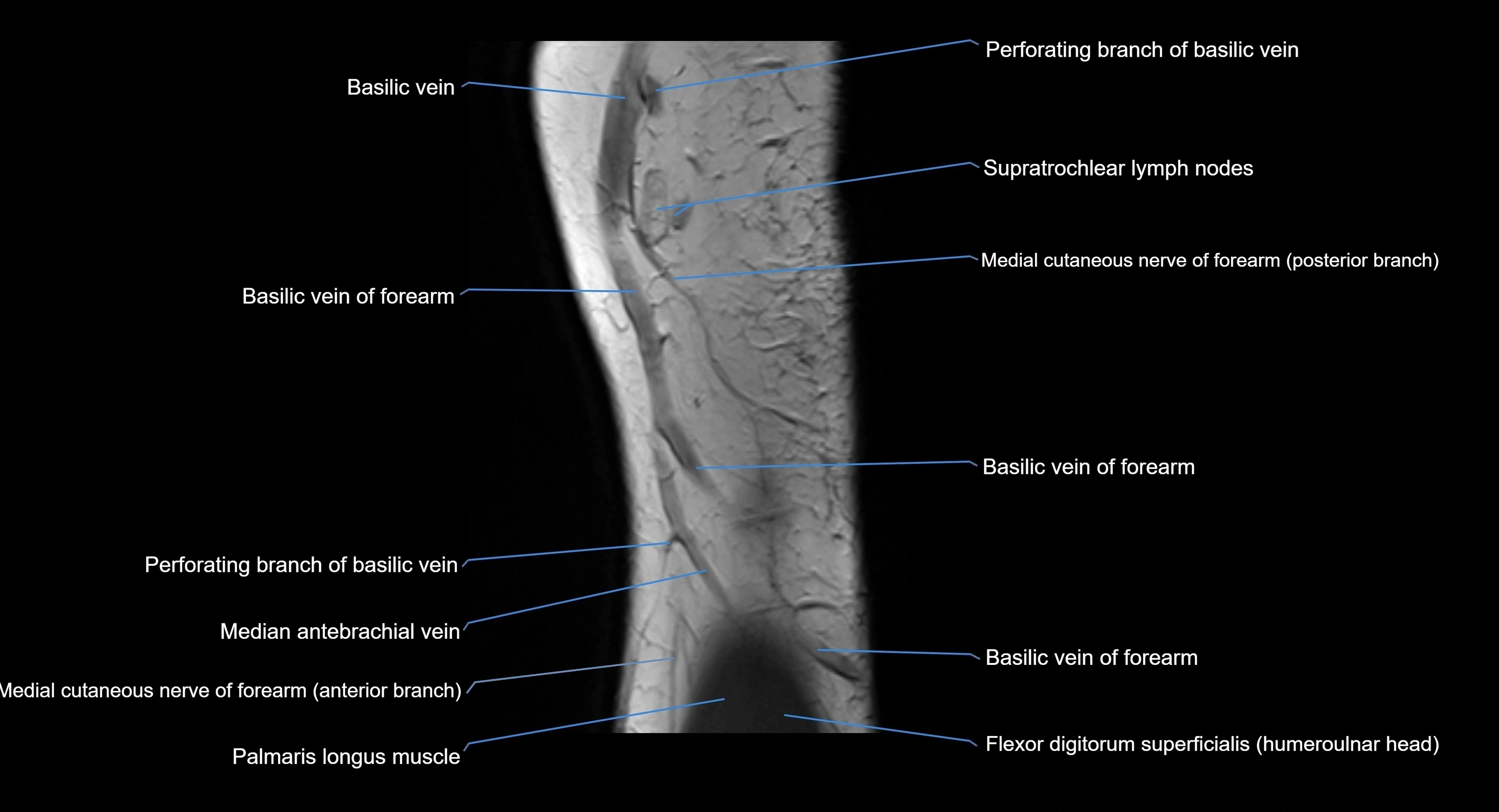
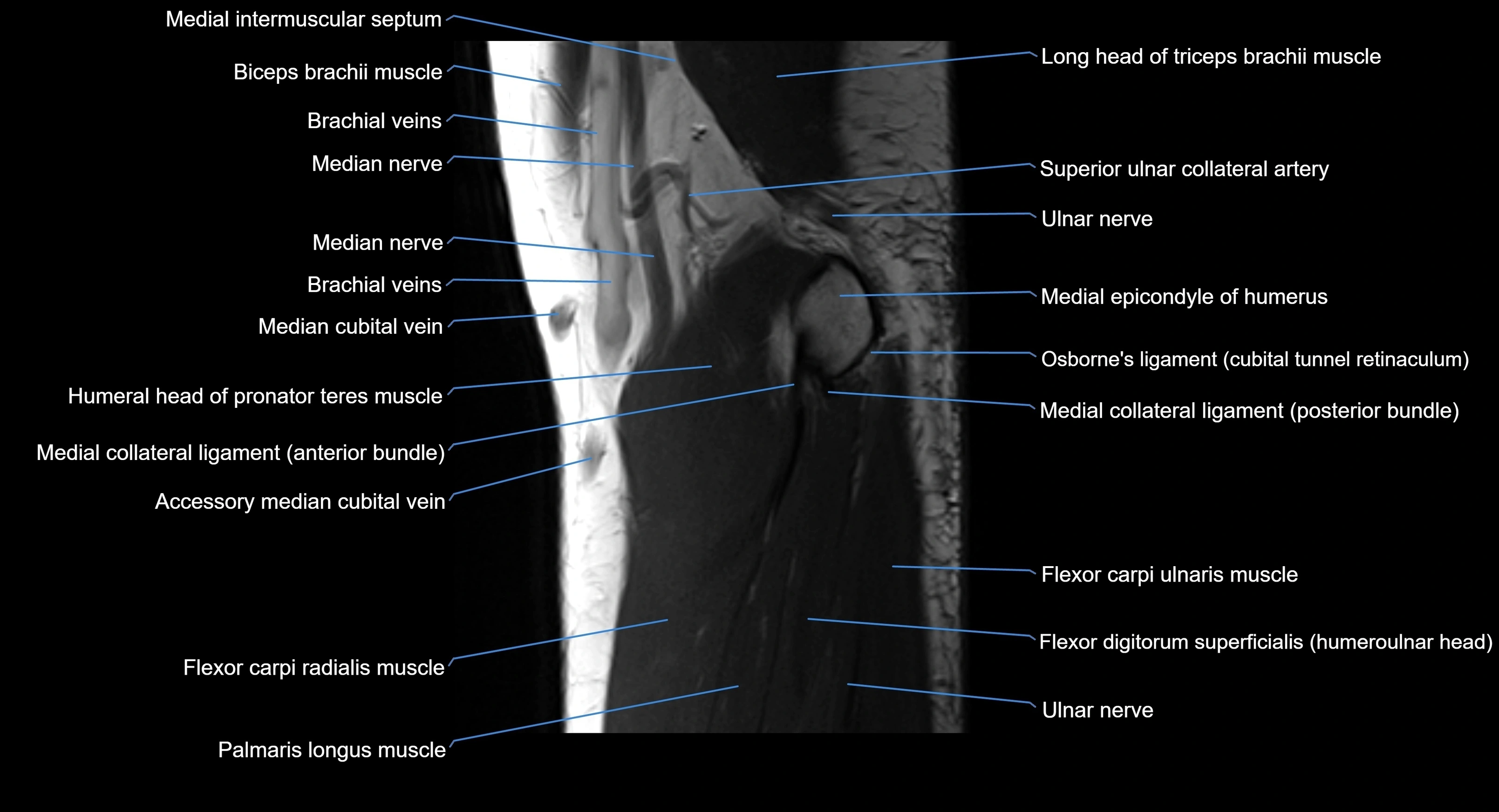
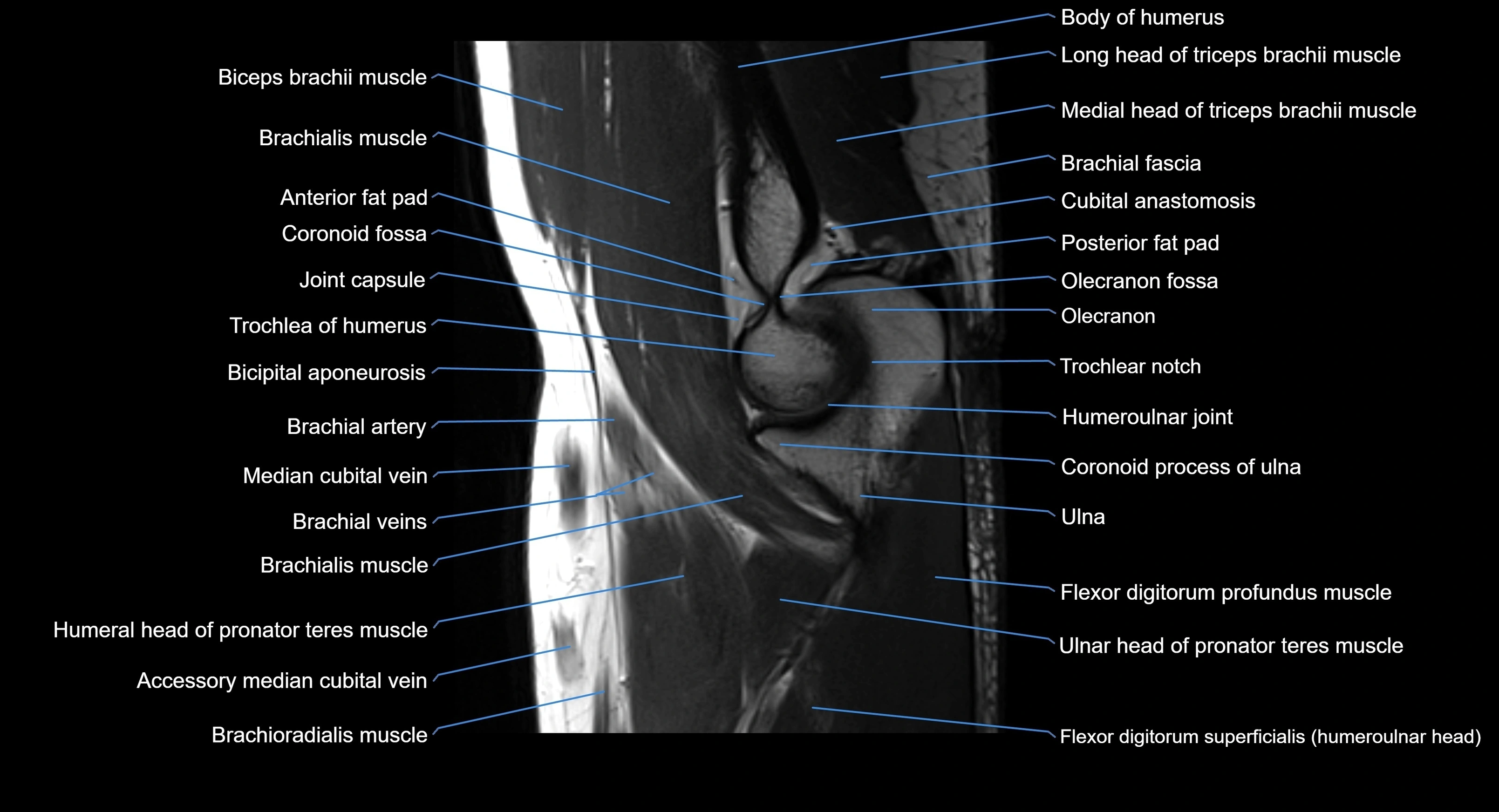
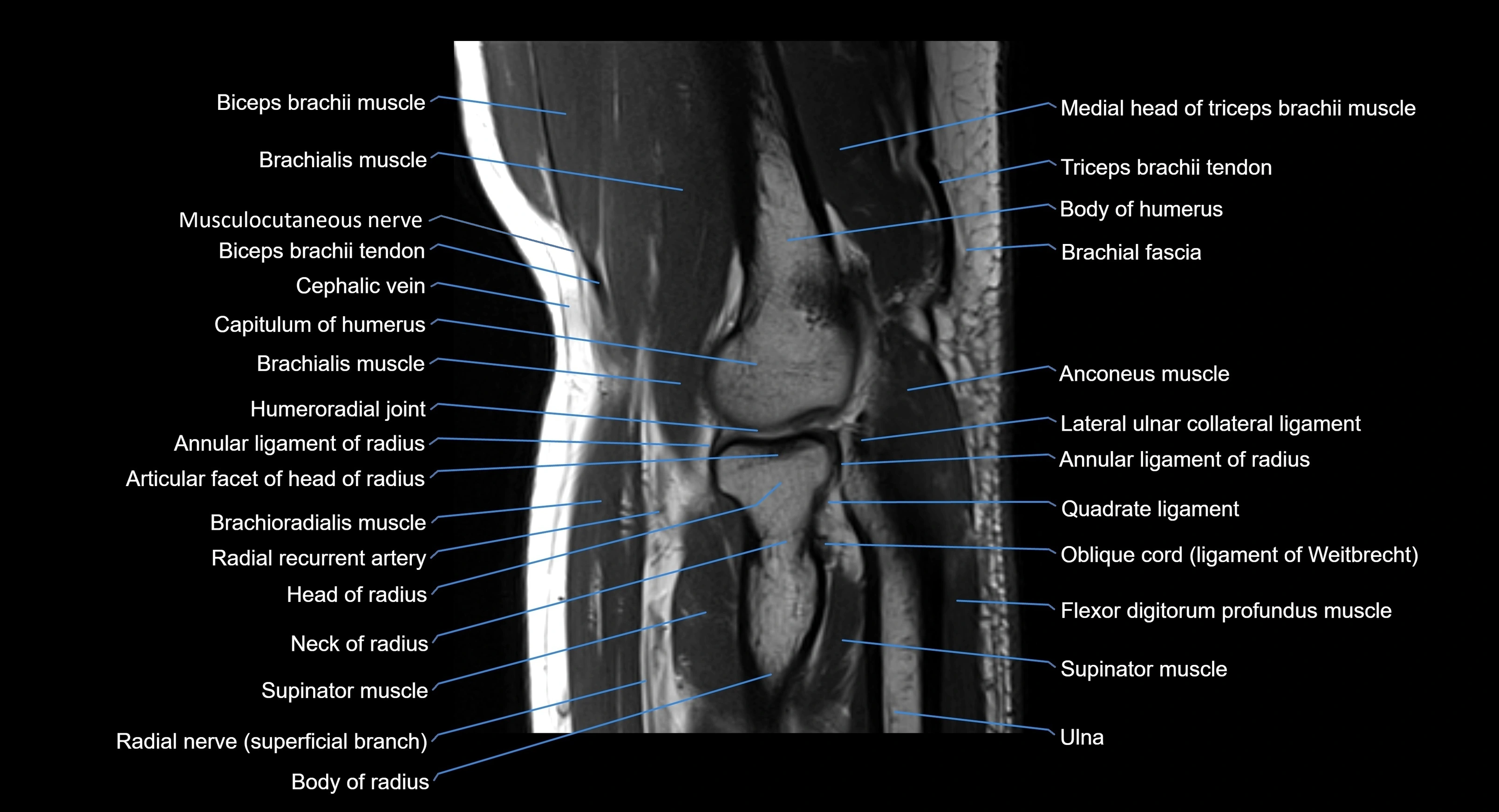
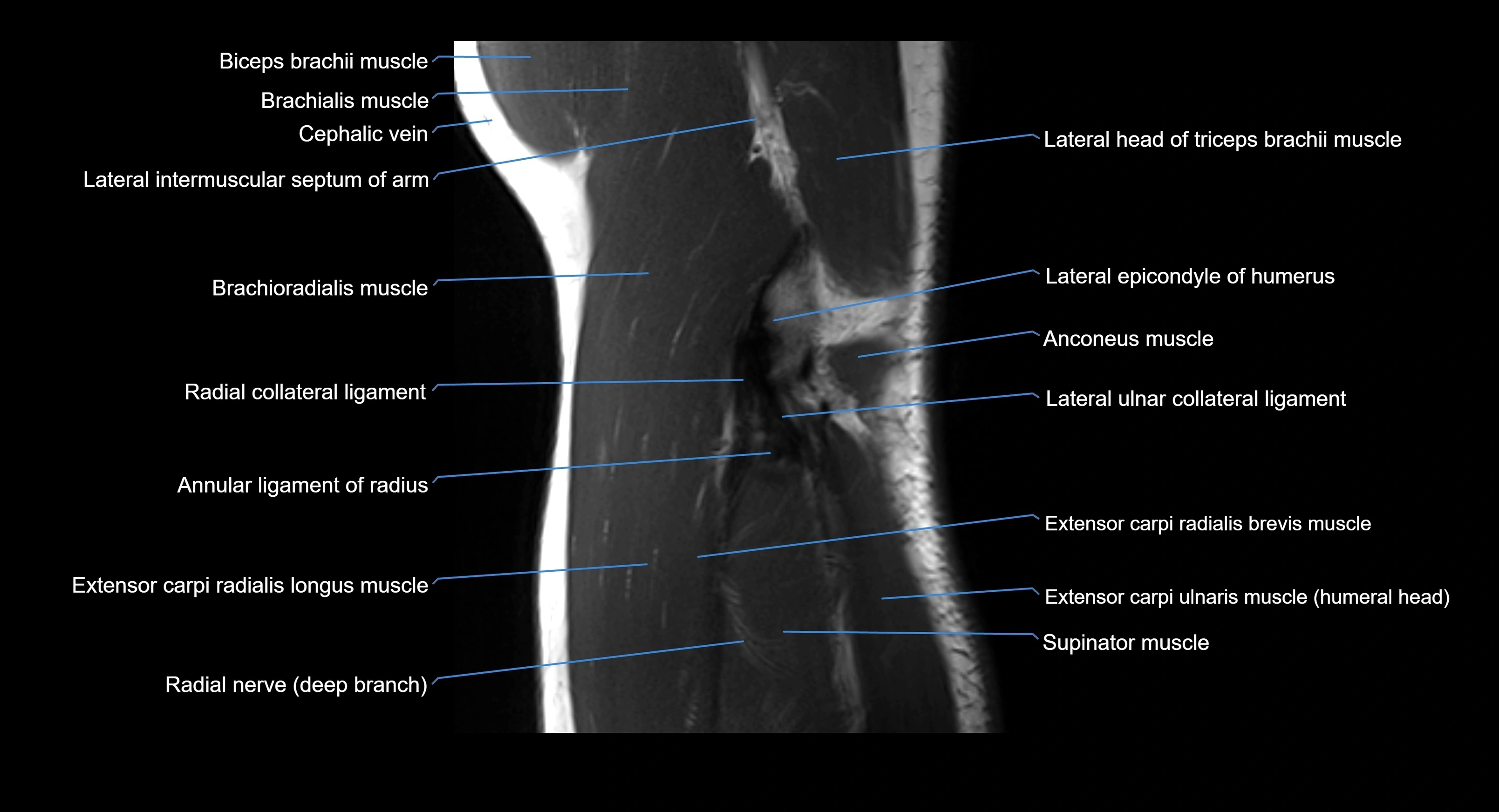
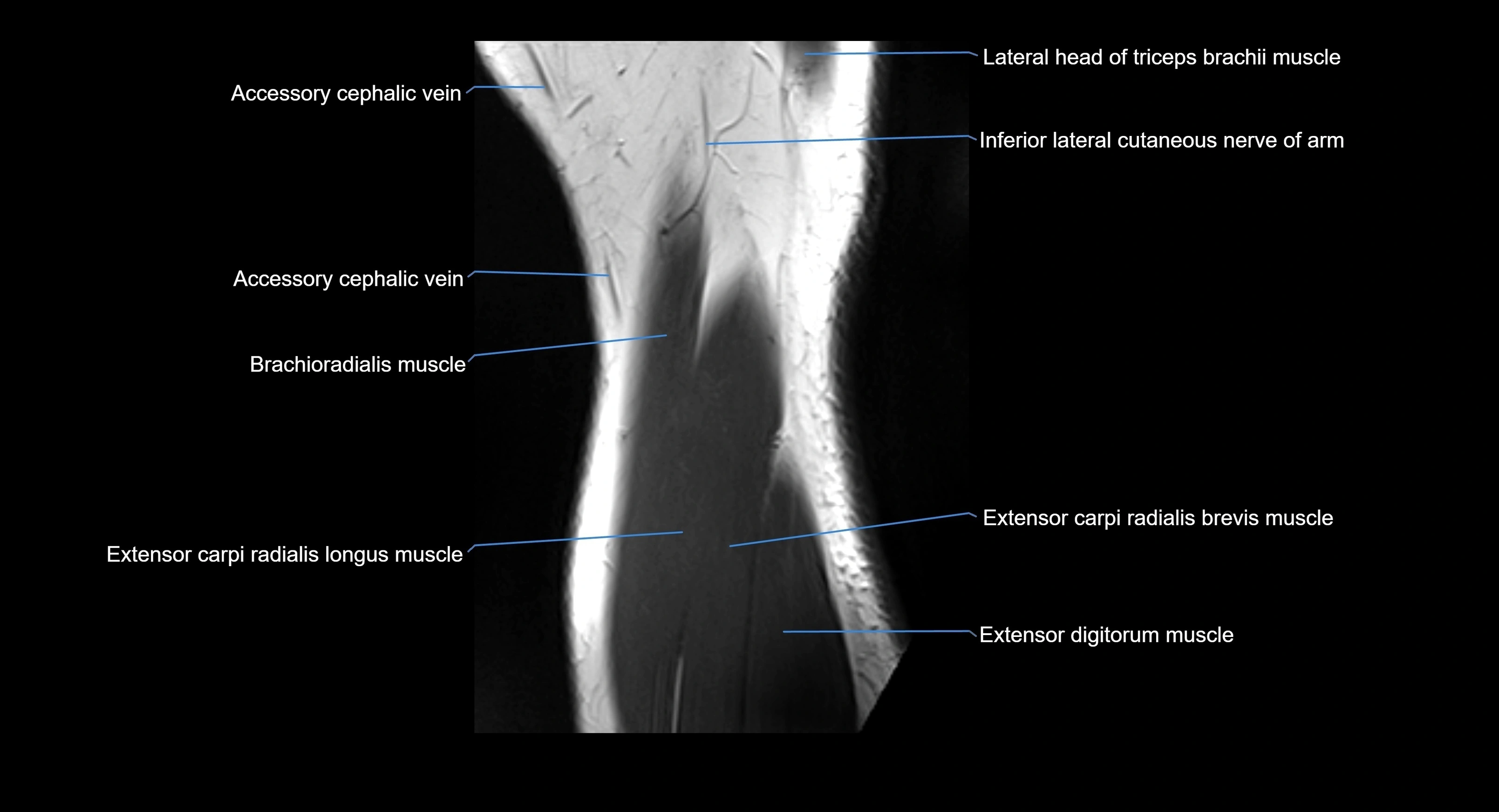
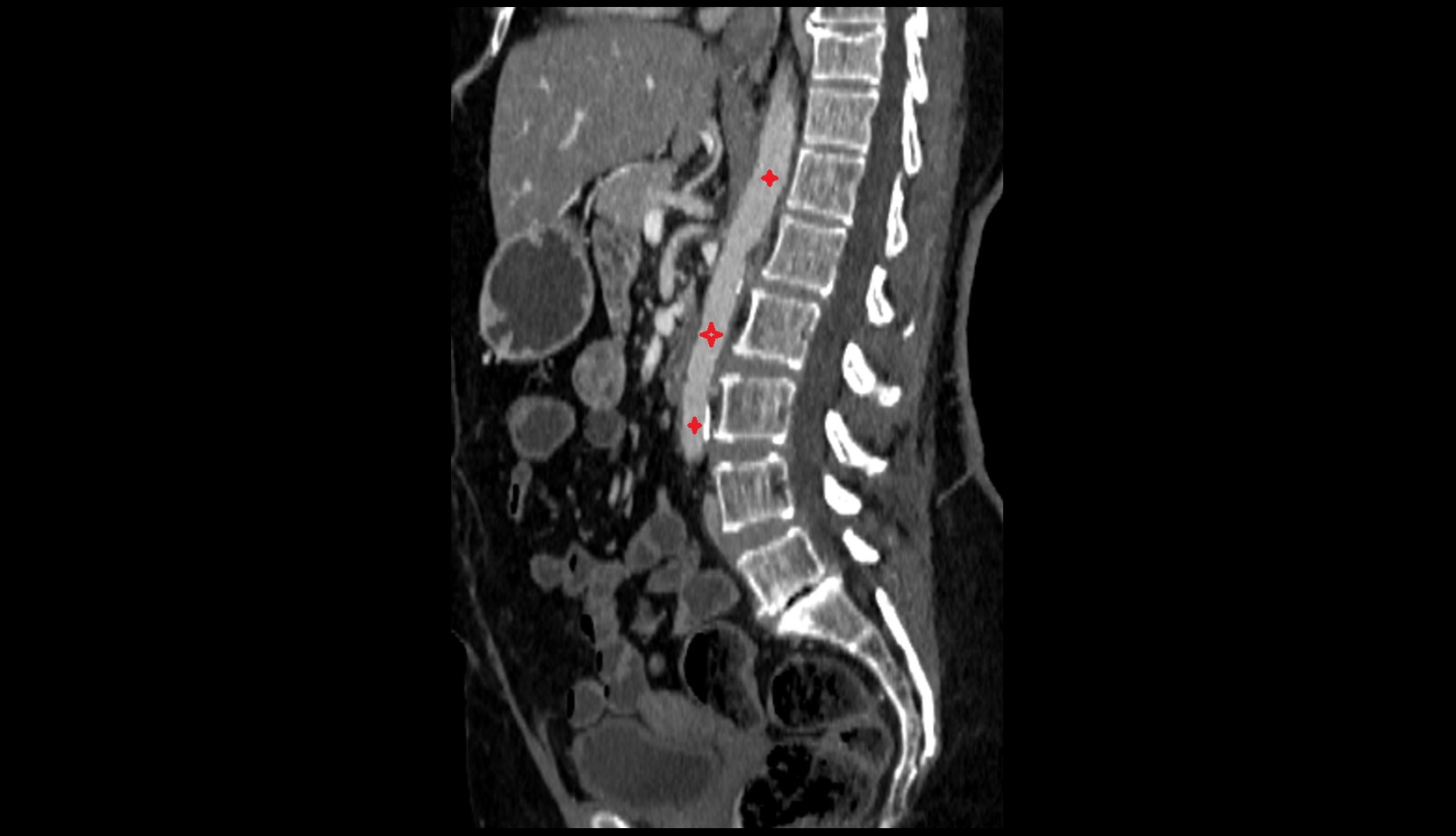
MRI image

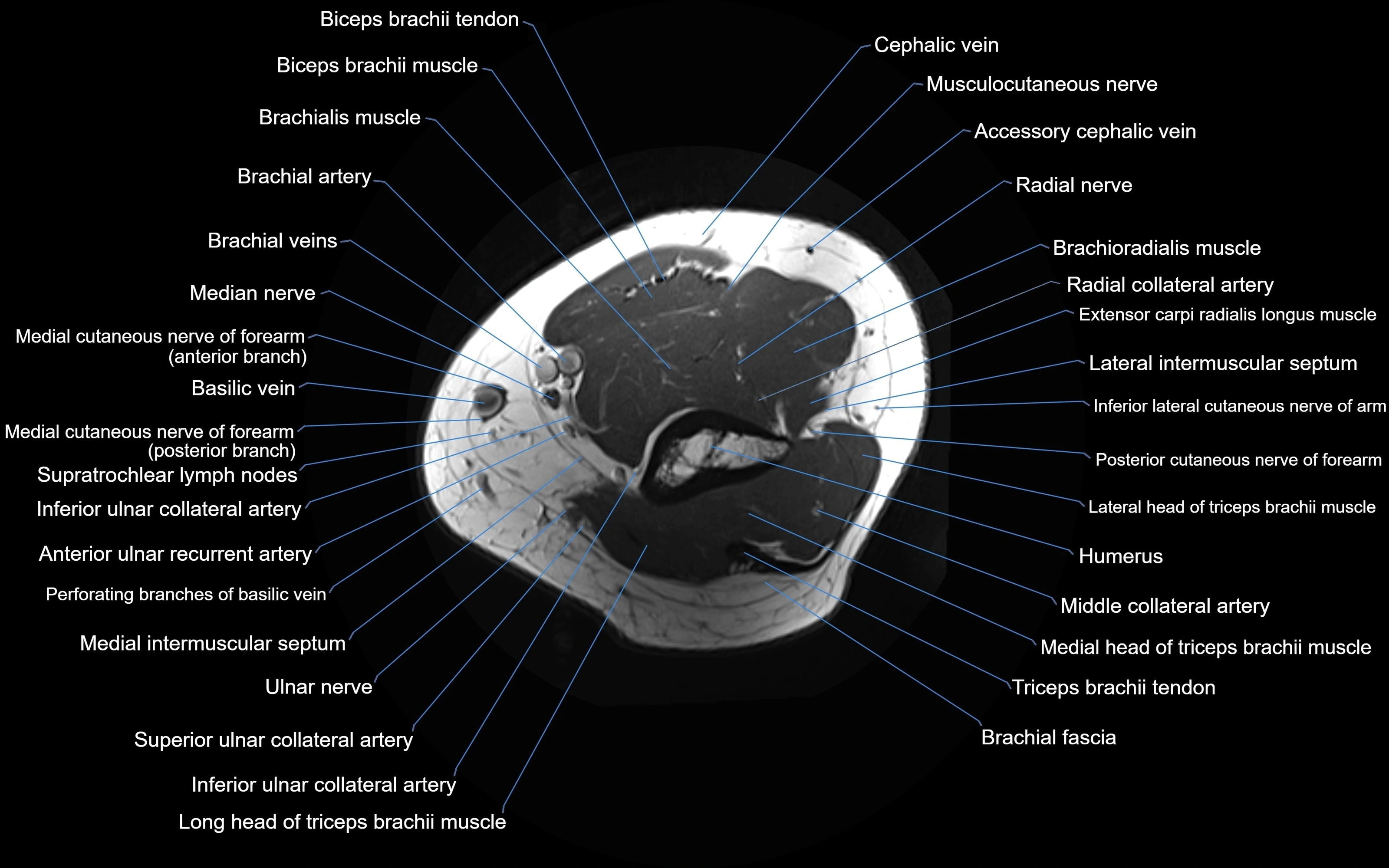
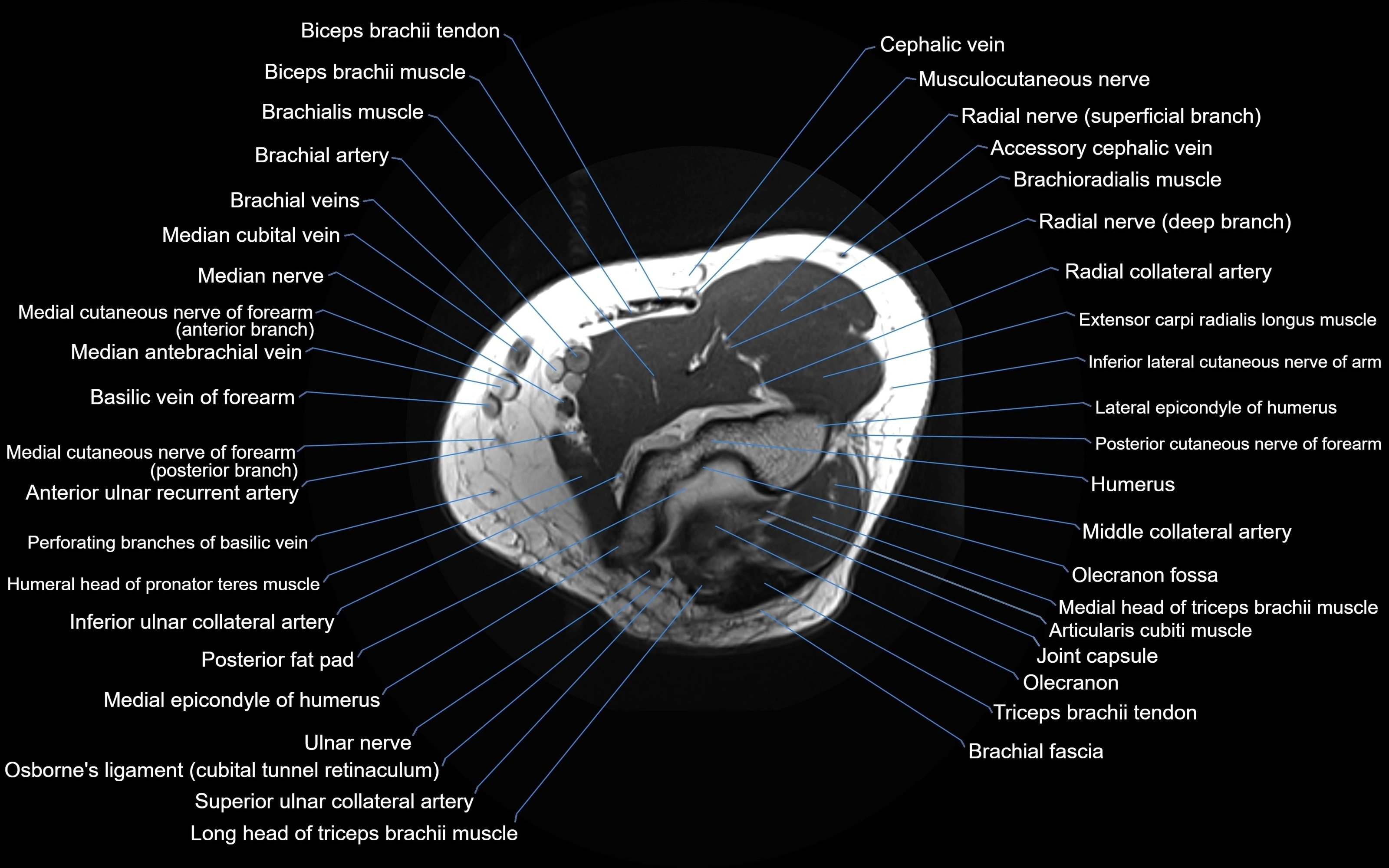
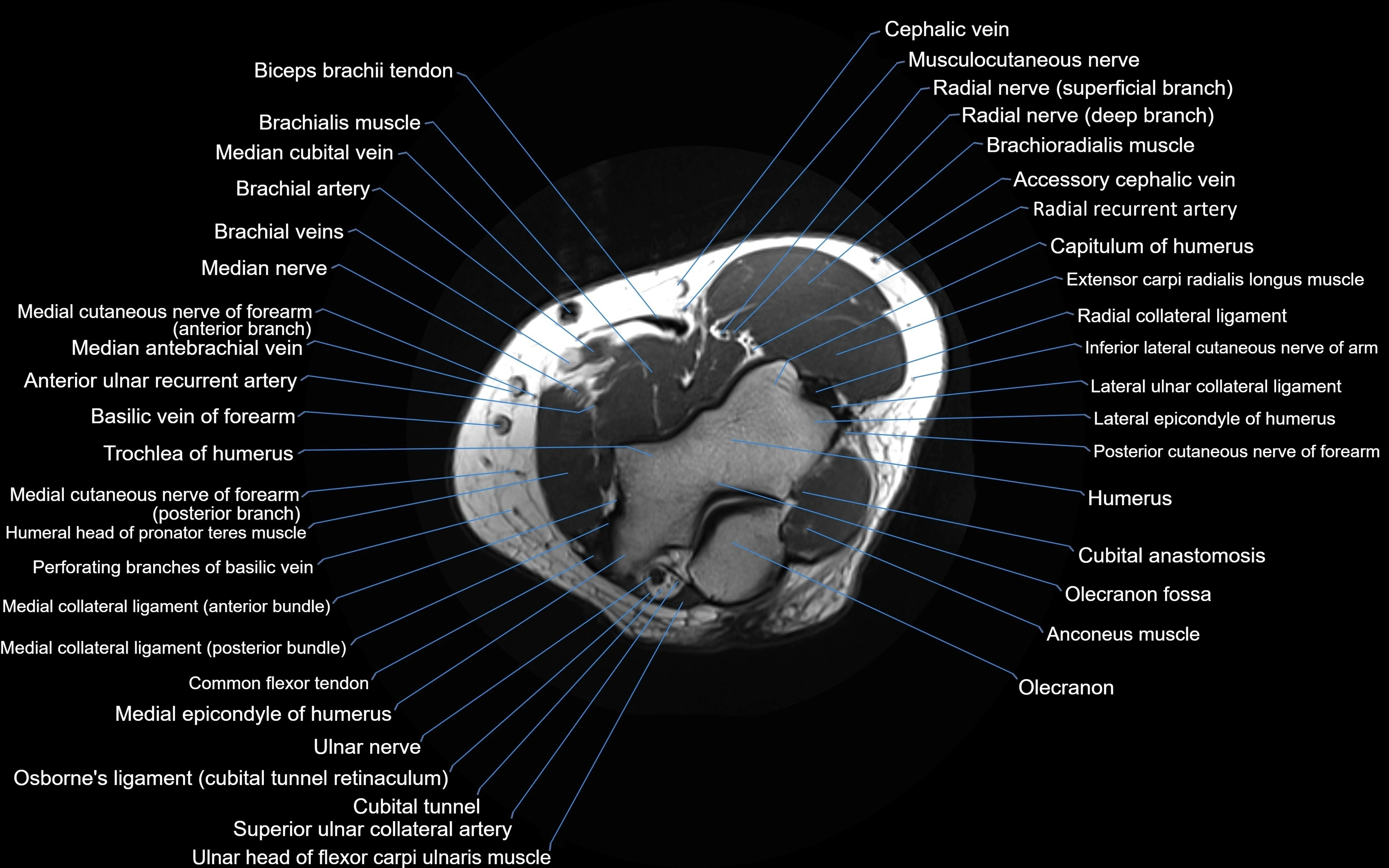
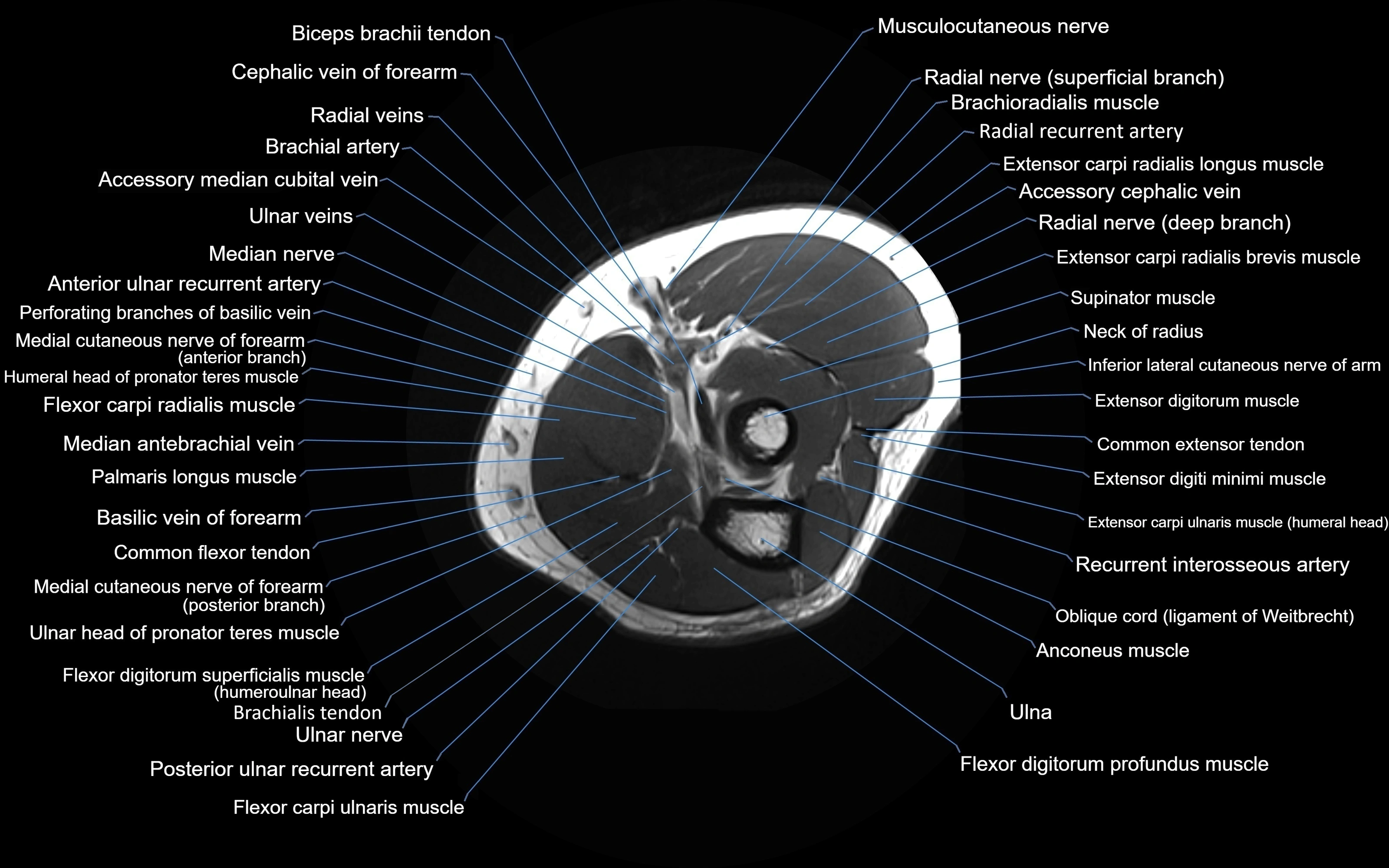
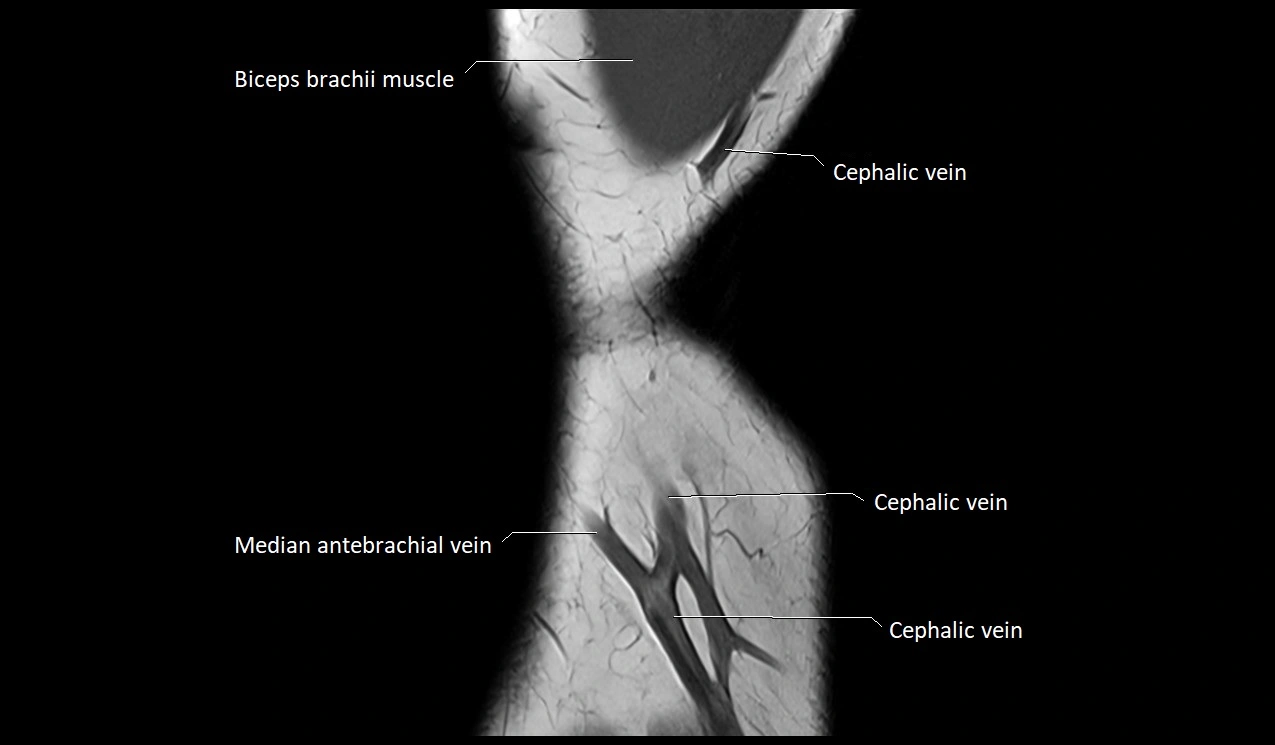
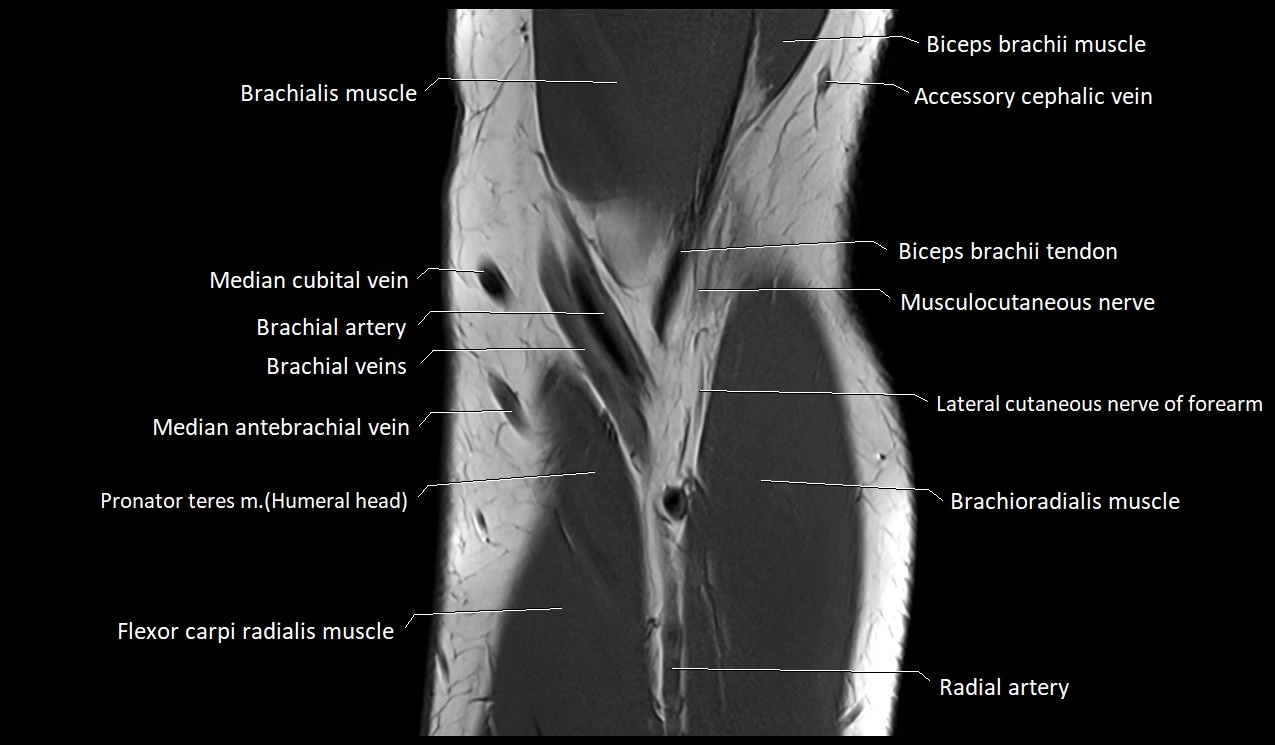
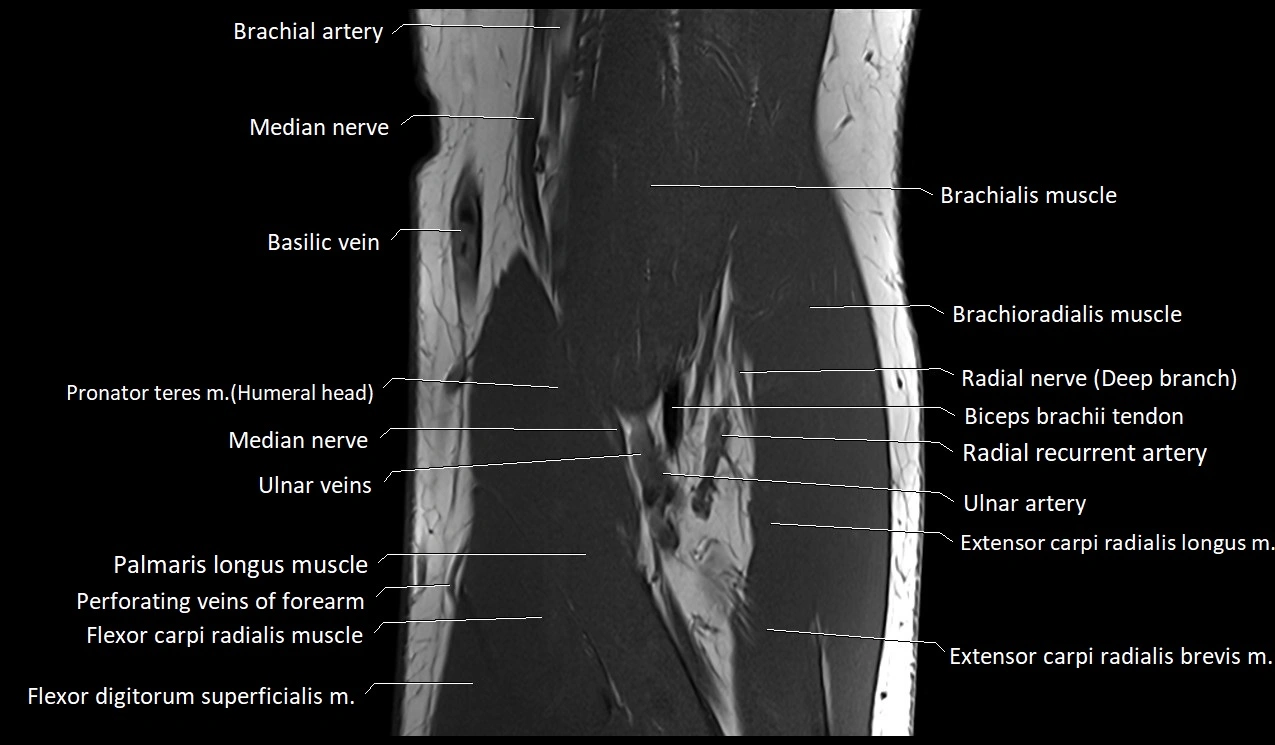
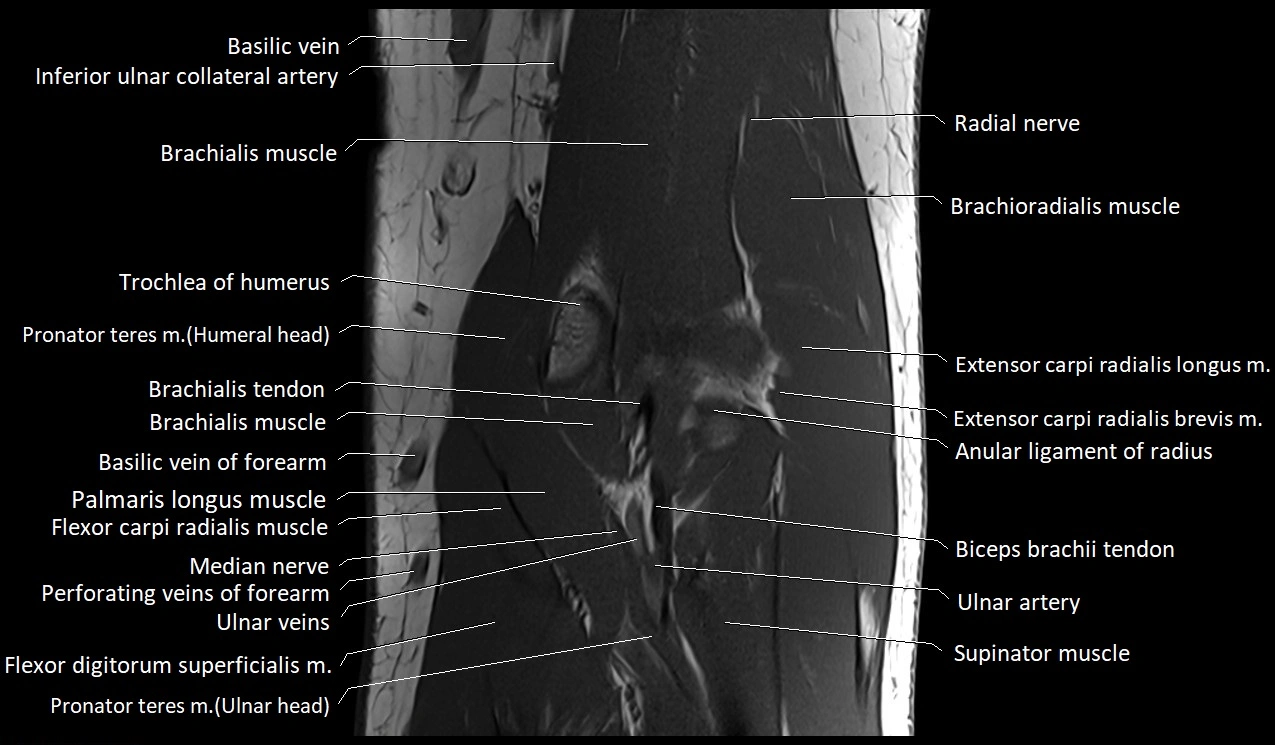
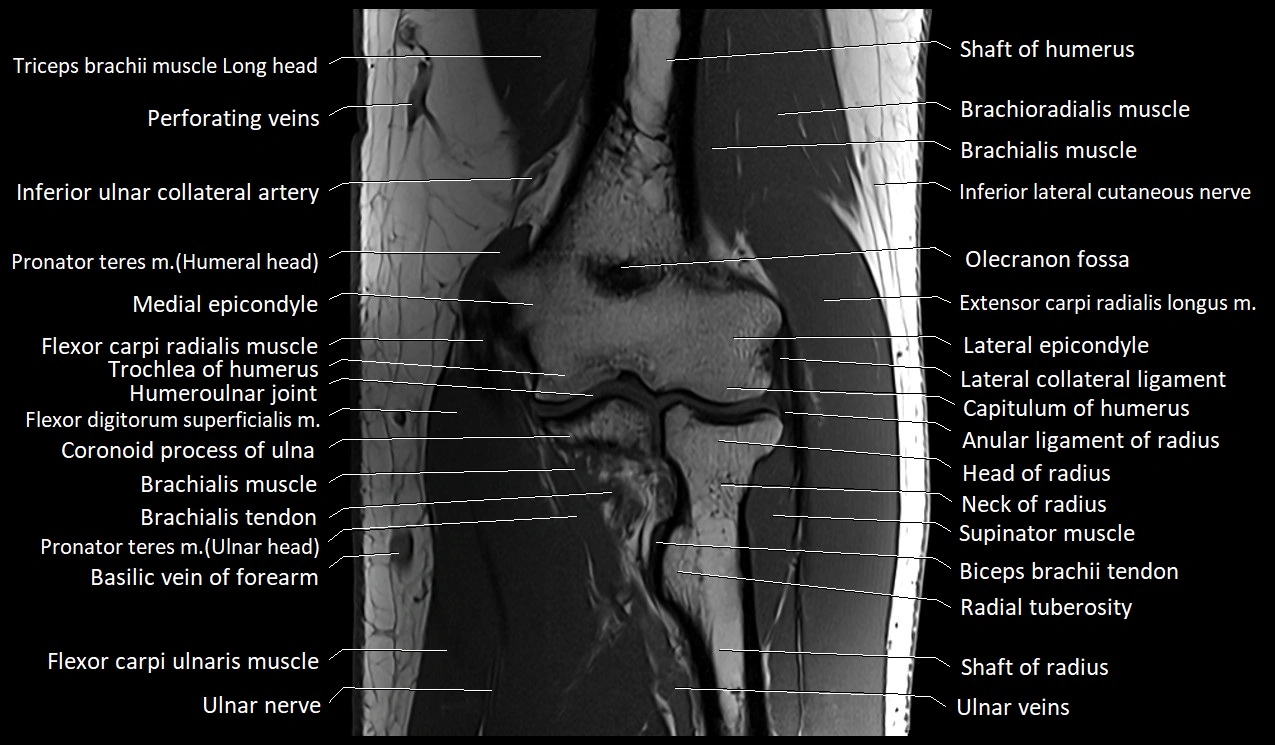
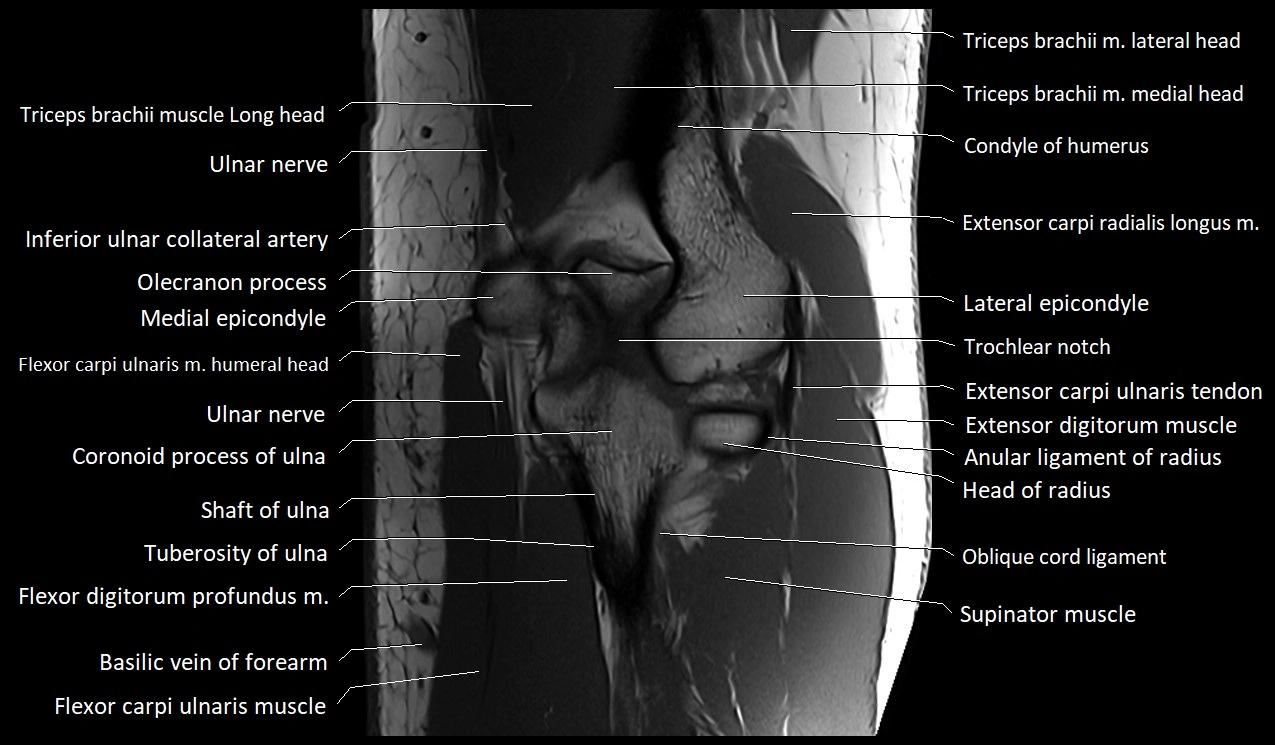
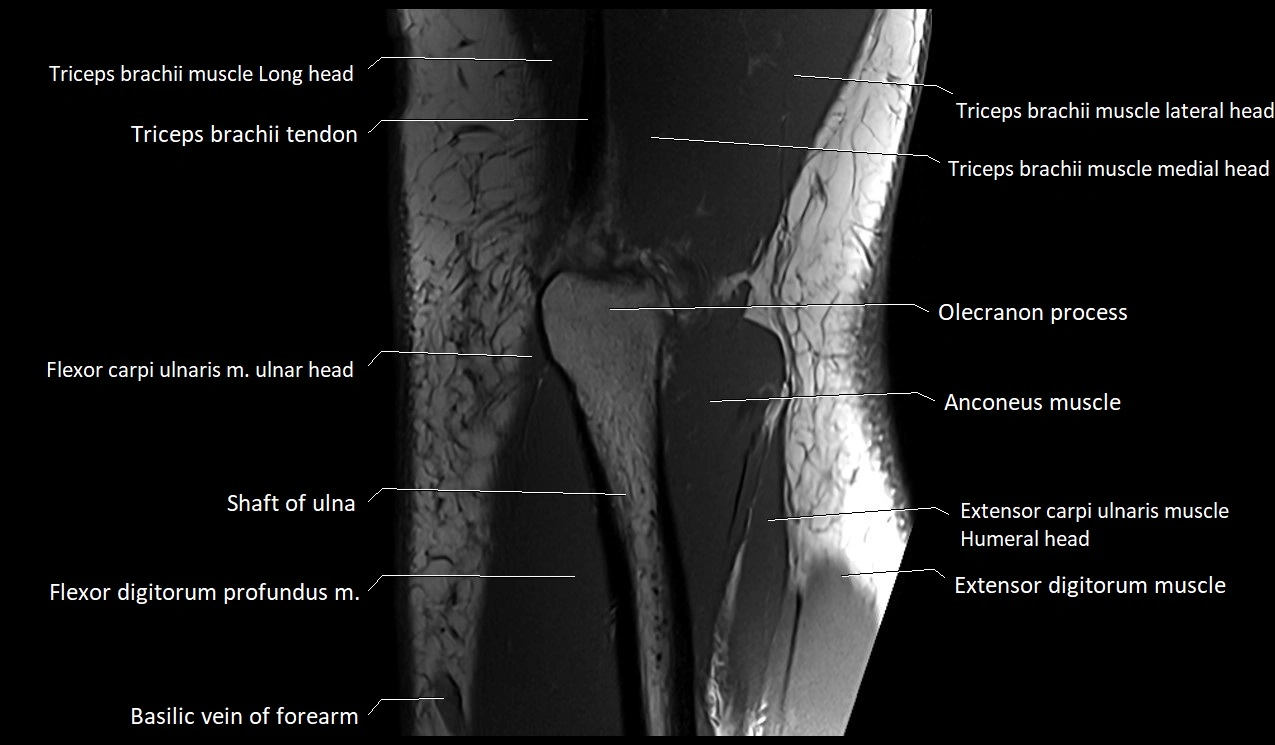
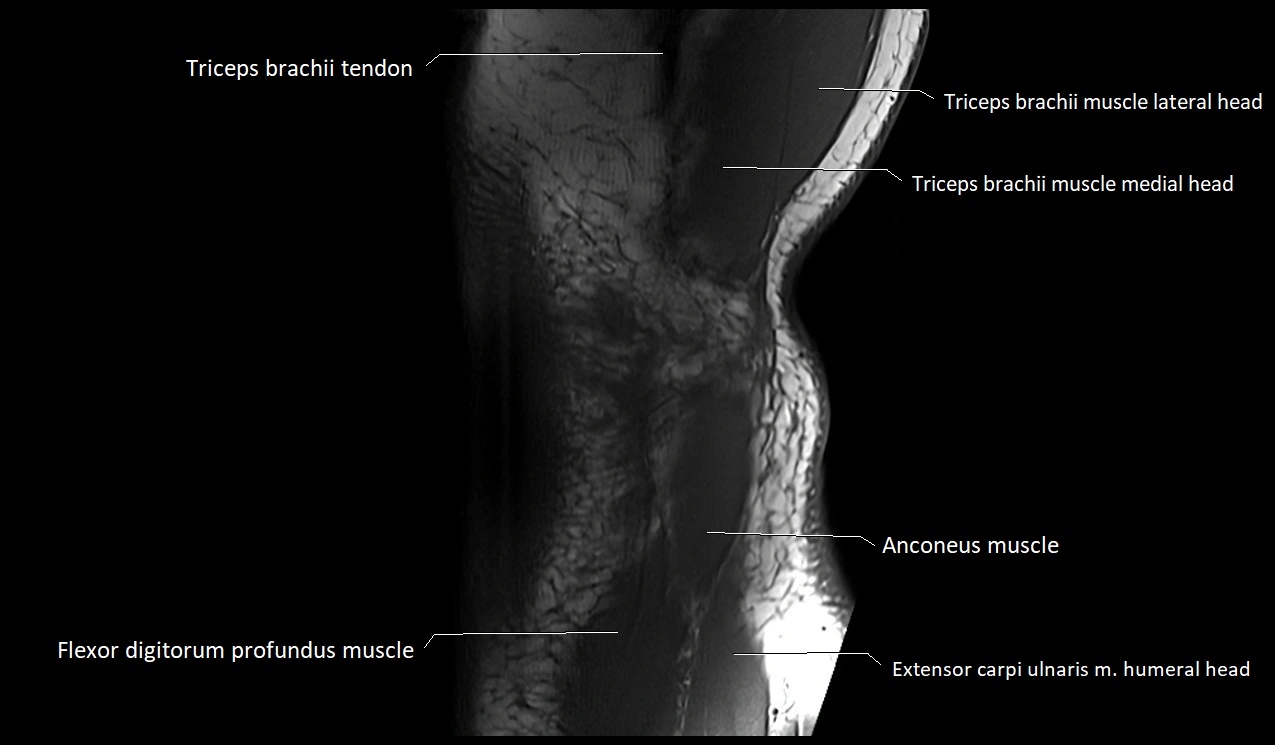
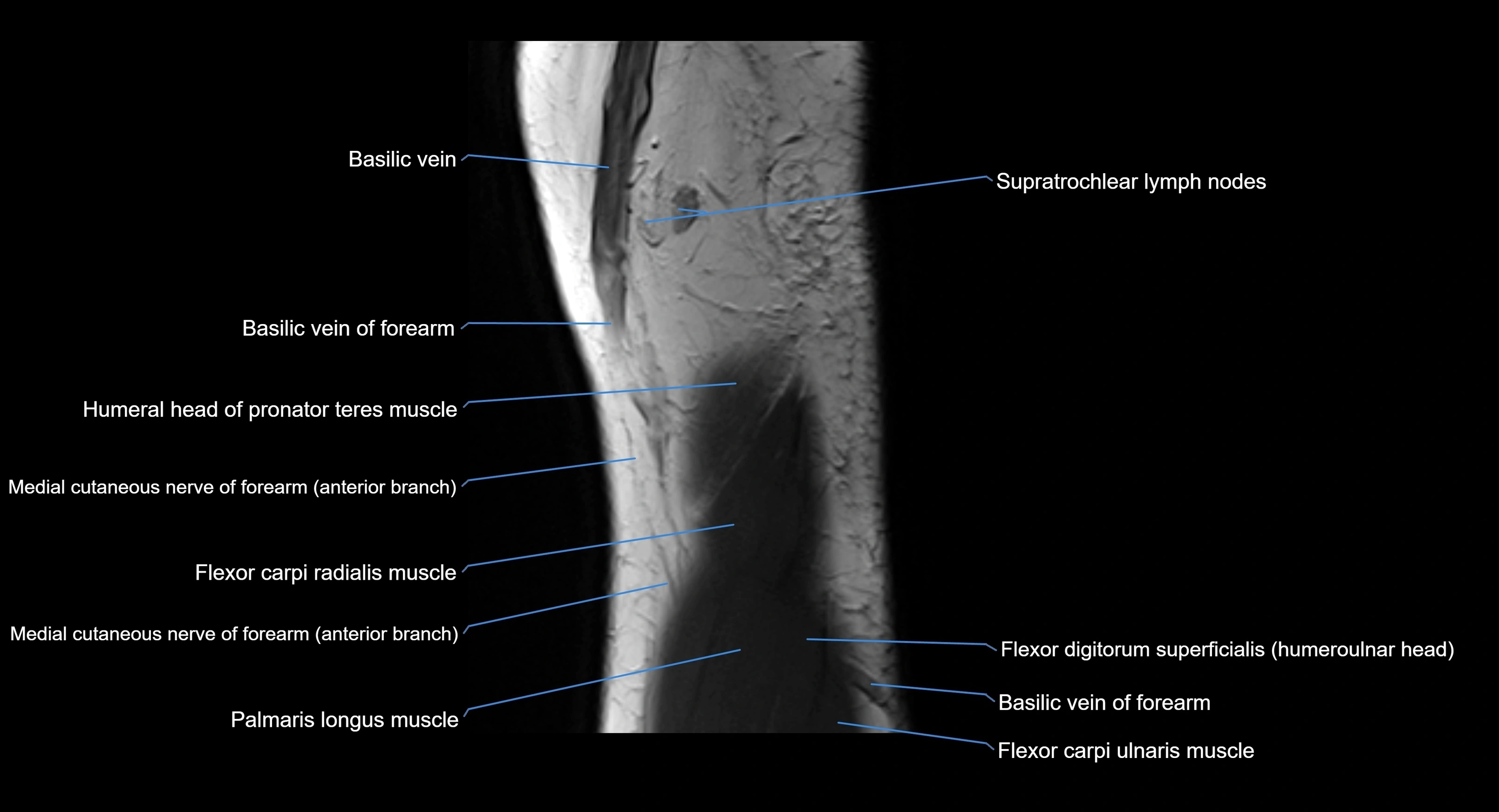
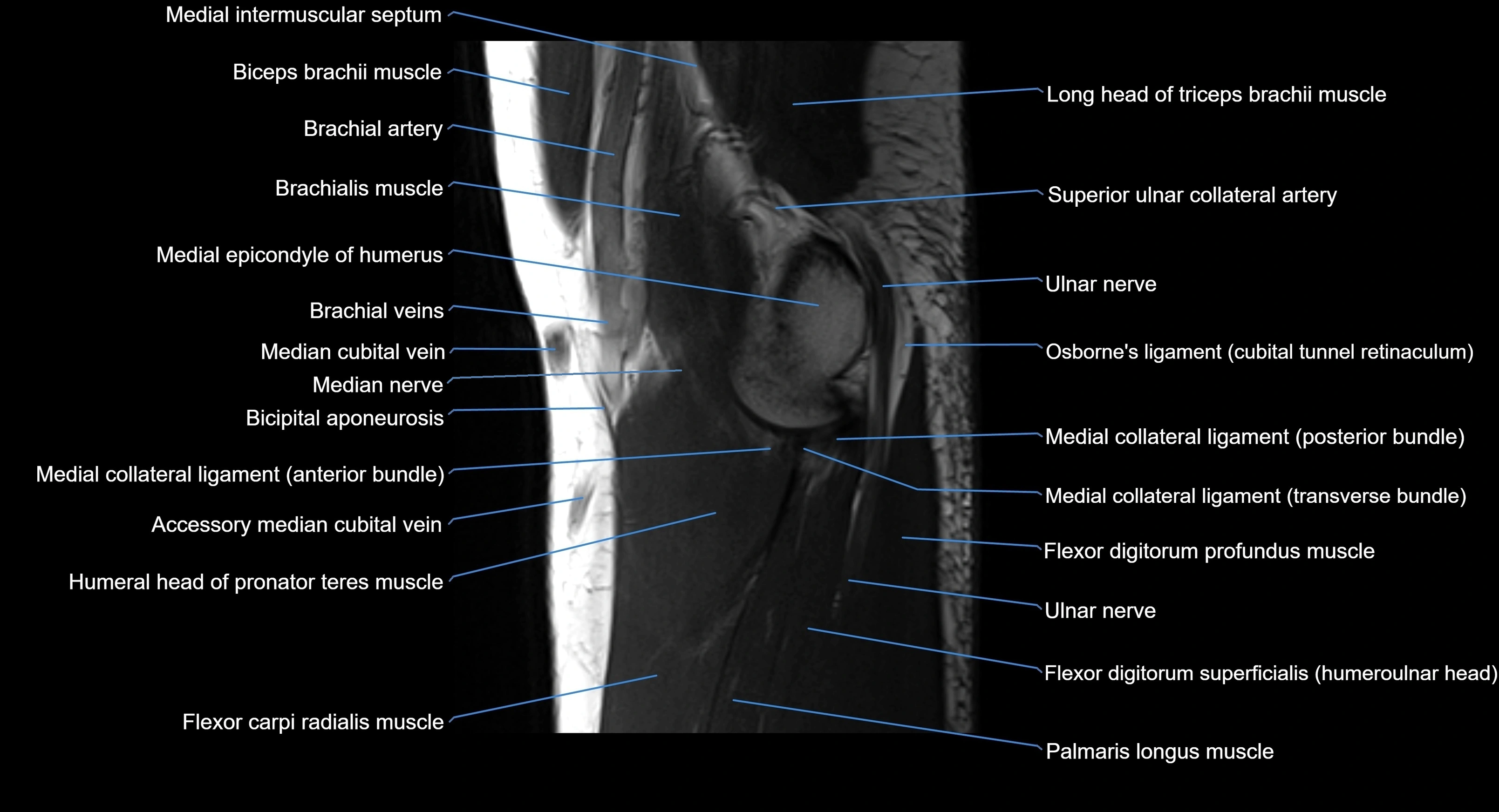
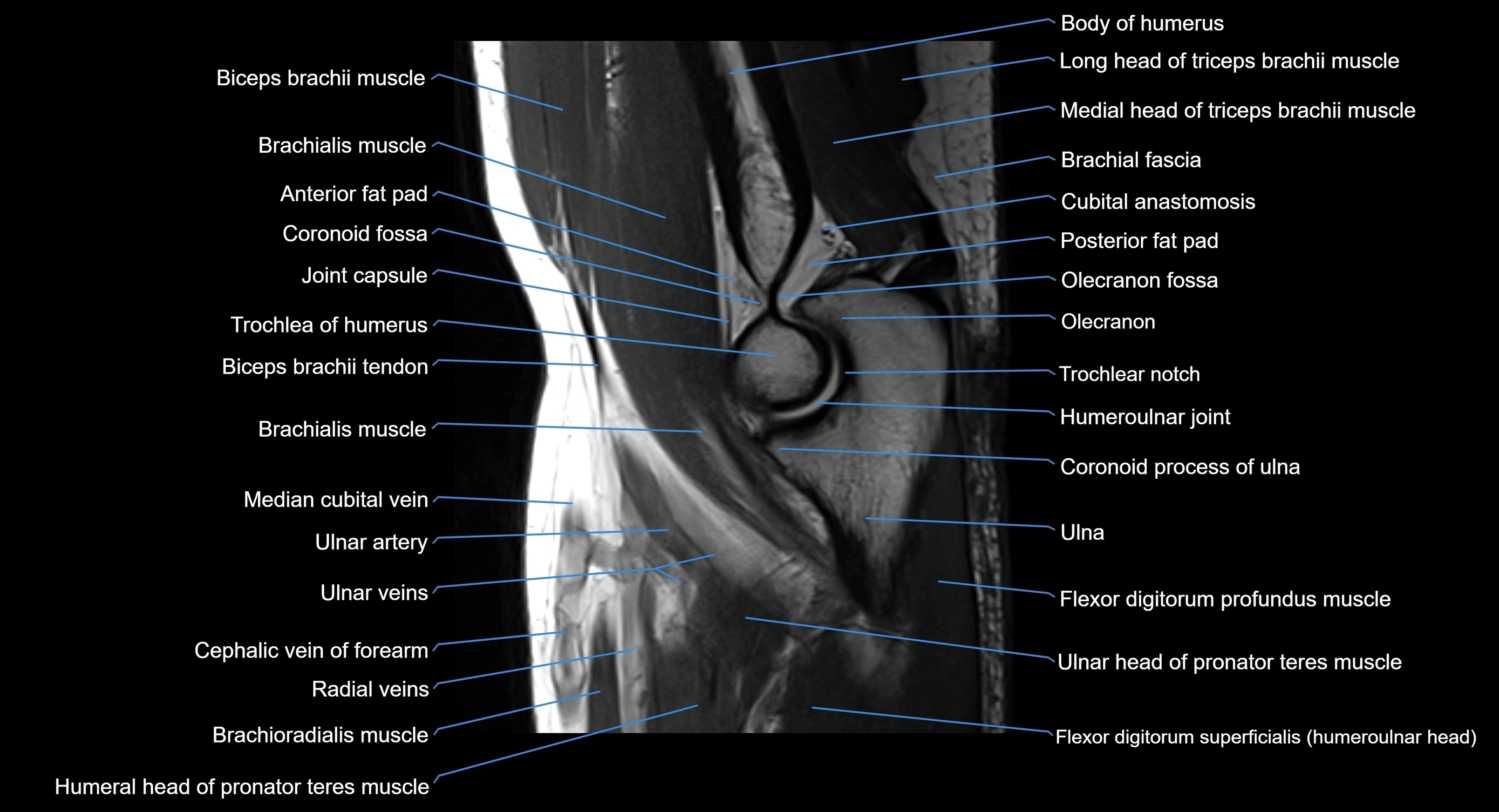
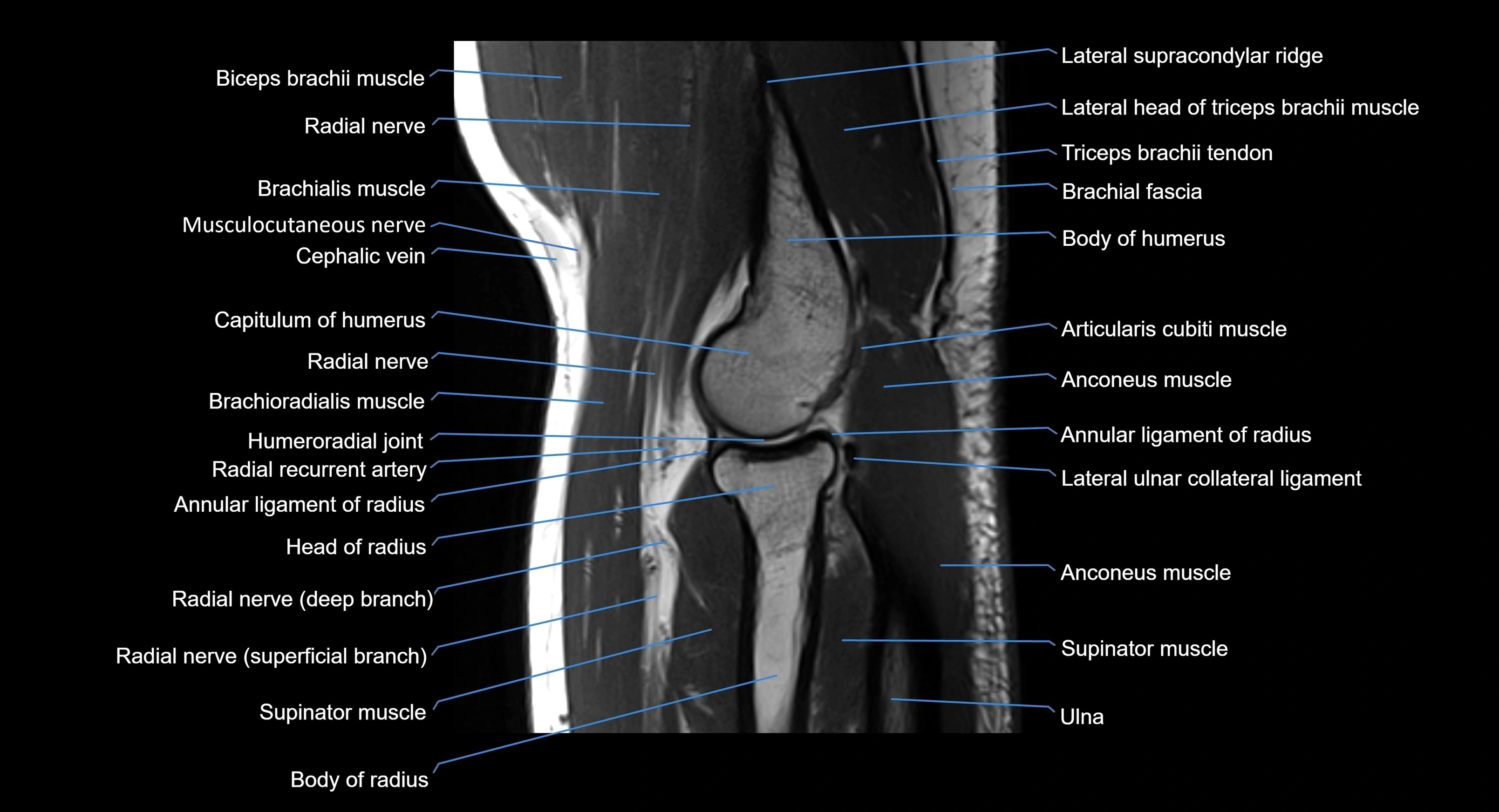
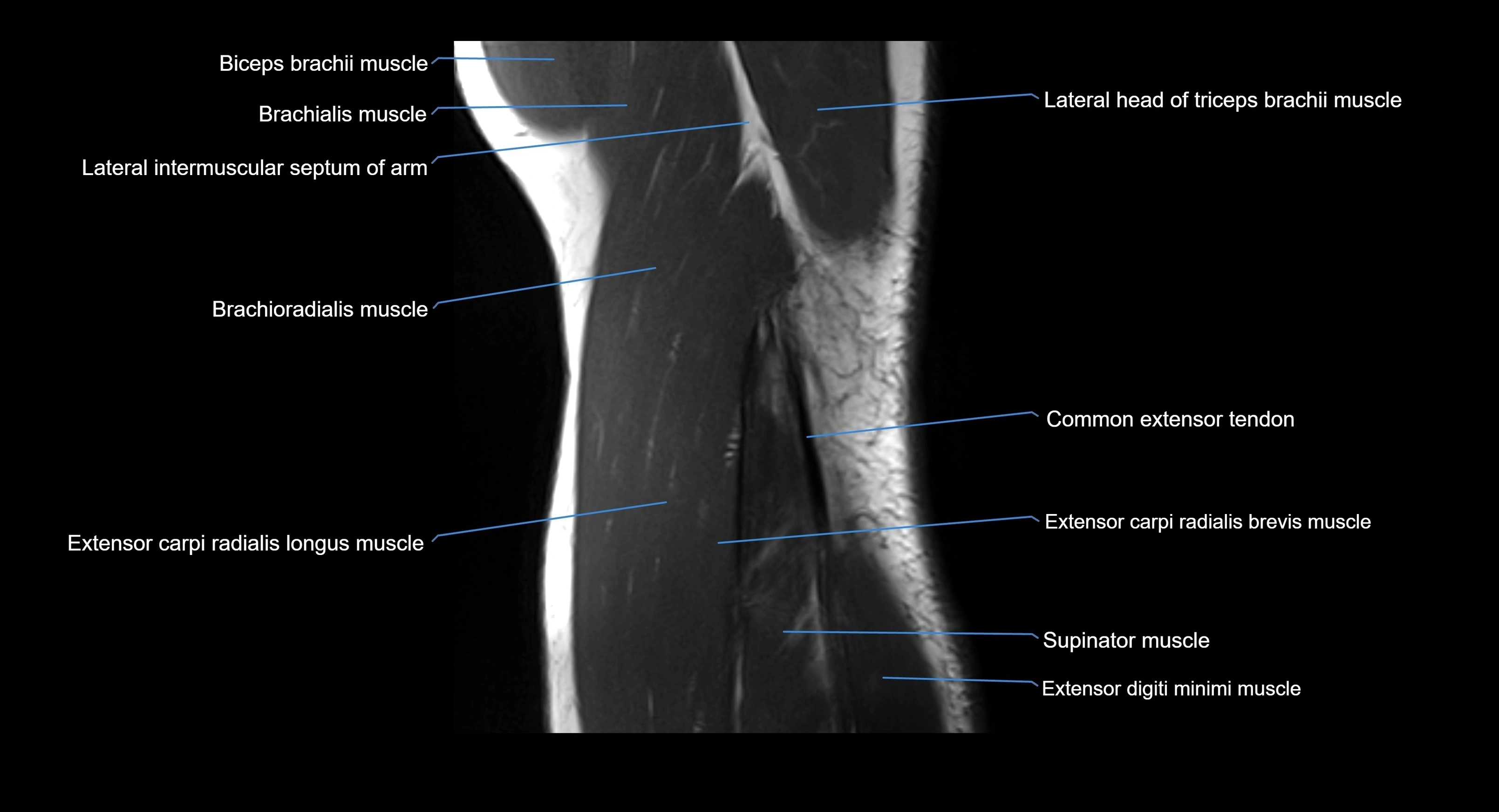
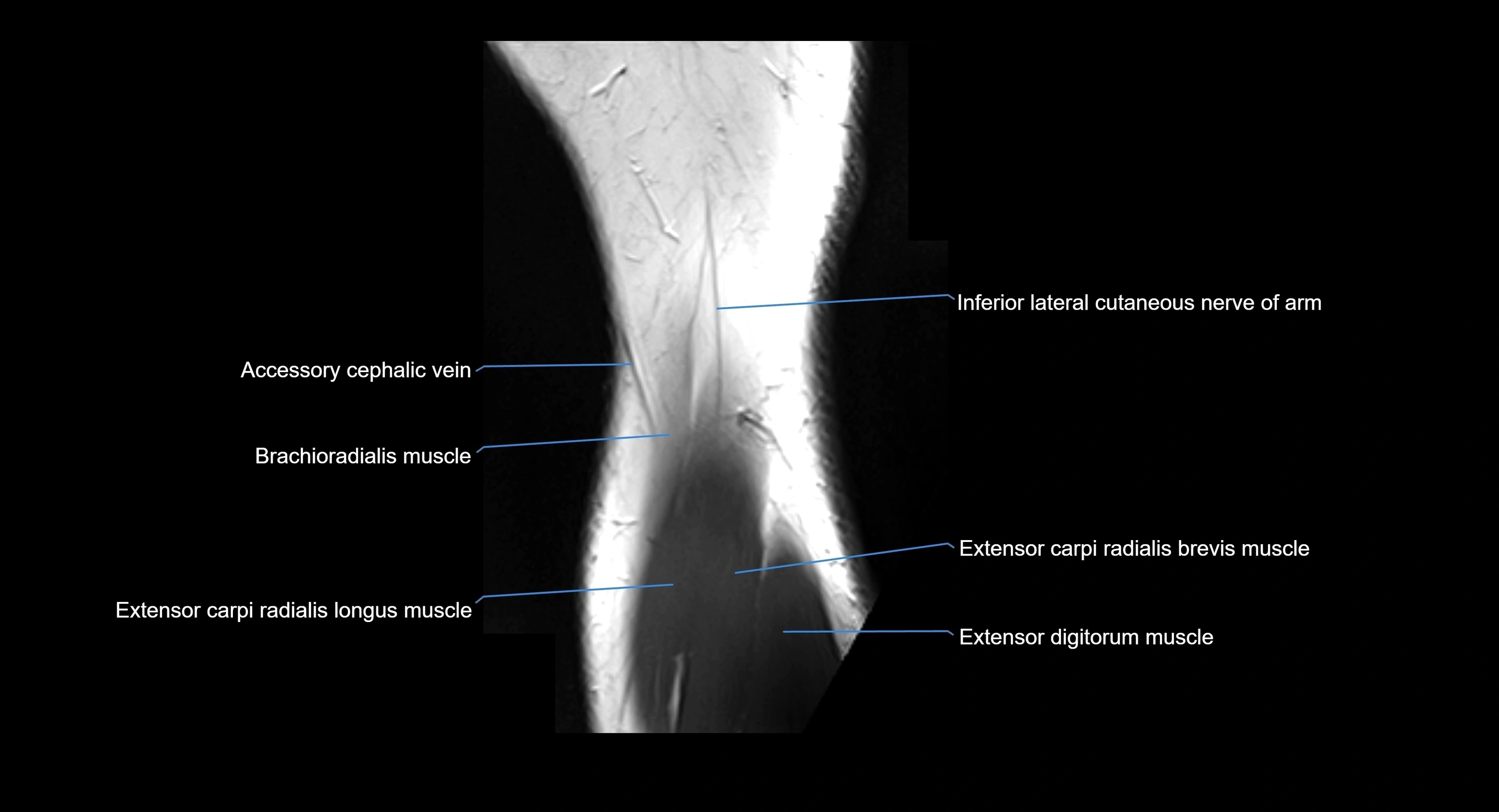
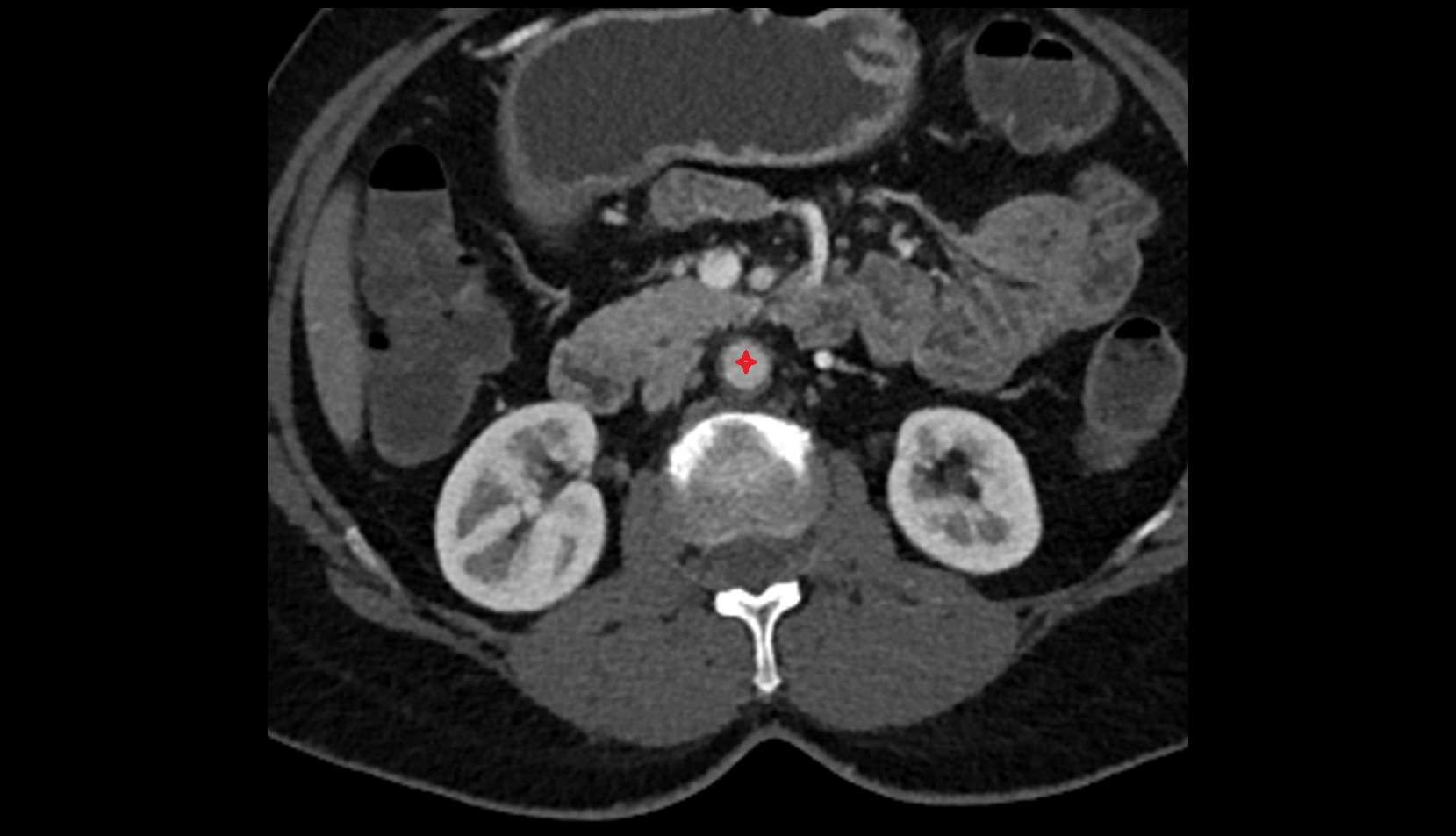
MRI image